The Ultimate Guide to Telehealth Technology
Introduction to Telehealth
Telehealth adoption is trending upwards due to higher uptake among healthcare systems and stronger demand from patients, on top of favorable regulatory changes. When successfully implemented as part of your healthcare strategy, telehealth technology can help you improve patient outcomes, reduce costs, and deliver quality care.
What is Telehealth?
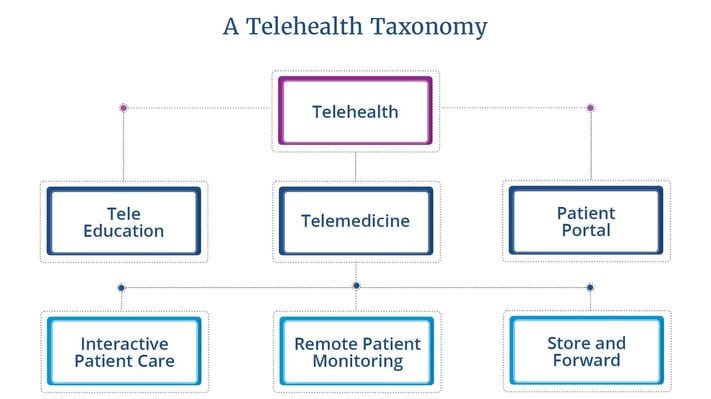
Terms like telemedicine and remote patient monitoring often crop up when discussing telehealth. While it may seem confusing, an easy way to understand the differences is to think of telehealth as an umbrella term under which telemedicine falls.
Remote patient monitoring, one of the central methods by which telemedicine is delivered, is nested further down the hierarchy.
Telehealth vs. Telemedicine vs. Remote Patient Monitoring
Telehealth
A broad range of technologies and services used to provide care and services at a distance.
Examples:
- Telemedicine
- Remote Monitoring
- Provider Training
- Non-clinical Training
- Prescription Delivery
- Health Education
- Provider-provider Education
Telemedicine
A type of telehealth that can be described as healthcare providers examining, observing, and treating patients at a distance.
Examples:
- Virtual Visit
- Medication Management
- Specialist Consultation
- Chronic Disease Management
Remote Patient Monitoring
A way to deliver telemedicine via “periodic, asynchronous, or continuous monitoring and transmission of vital signs.”
Bluetooth biometric devices record:
- Weight
- Blood Pressure
- Oxygen Saturation
- Glucose Levels
- Heart Rate
- Heart Rhythm
How Telehealth Technology Works
For telehealth to be sustainable and scalable, it’s important for the telehealth software to have cloud-based functionality. What cloud-based telehealth services enable is secure, anytime access to medical records for both healthcare providers and patients as long as they are connected to the internet.
A HIPAA-compliant cloud-based telehealth platform ensures confidentiality and prevents personal patient information from being disclosed without consent. For example, the solution may offer messaging tools that are encrypted for security, and allows physicians to interact with and monitor their patients through a cloud-based dashboard.
The tools or features within a telehealth program can be categorized into asynchronous and synchronous telehealth. Both categories offer impressive benefits to patients and providers and in some specialties, one form could be more effective and efficient than the other.
Asynchronous telehealth can be simply defined as a “store-and-forward” communication between parties that is not happening in real time. While applicable across a broad range of specialties, it may be particularly helpful for departments like dermatology, radiology, orthopedics, ophthalmology, and cosmetic surgery.
Synchronous telehealth is the opposite in the sense that it happens in real time, oftentimes via virtual visits that are carried out over video call. It facilitates in-depth patient-provider interaction and allows the provider to enquire and communicate about the patient’s care and condition.
 Quick facts: Synchronous telemedicine
Quick facts: Synchronous telemedicine
- In a study comprising 650 patients, 74% reported that they had their care concerns resolved on telemedicine visits with synchronous audio and video on demand.
- Each emergency department visit that was avoided due to synchronous telemedicine resulted in cost savings ranging from $309 to over $1,500.
- In a survey targeting 1,274 patients who had a video visit over three months, 84% responded that video visits improved their relationship with their provider.
Evaluating Telehealth Companies
There are three key areas to consider when evaluating telehealth vendors:
- The telehealth platform
- The telehealth provider
- Telehealth equipment
What to Look for in a Telehealth Platform
The telehealth software and its capabilities will help you drive your healthcare strategy and initiatives. Ultimately, it should help you streamline and save time on existing processes. Here are some features to look out for:
- Bluetooth biometric remote monitoring
- Real-time video calls, phone calls, and texting
- Medication alerts
- Condition-specific education
Getting the Best Telehealth Services
To maximize the potential and sustainability of your telehealth program, look for a telehealth provider that can act as a long-term partner to your organization. Take your time to ask questions about the scope and duration of their support, and what your industry peers have to say about their telehealth services. Think about the following considerations:
- Cost
- Support services
- Clinical and reimbursement
- Results
- Implementation and account management
Expanding with Telehealth Equipment and Remote Patient Monitoring
Telehealth technology includes a wide range of tools and devices that can be customized depending on your needs. Examples include telemedicine technology for virtual visits and patient education, like tablets and mobile phones; or Bluetooth biometric devices that record daily vitals.
The range of telemedicine technology you can deploy can be overwhelming, so begin by identifying the components that you want to include based on what would best connect your patients to healthcare practitioners.
At the core of it, you have a telehealth platform operating on a device that’s used for communication and gathering data from telehealth monitoring devices. Whether you add on more components or simplify depends on the level of engagement and care required.
Inventory management is crucial to success at this point and for a start, you can establish the following best practices to create greater efficiency for your team and the program:
- Equipment tracking
- Unit storage
- Creation of a telehealth procedure manual
Final steps: Putting together a telehealth program
There are many things to think about when planning your telehealth strategy, especially if you’re starting from scratch. Success is dependent on various factors like establishing clear objectives, choosing the right telehealth partner, and getting buy-in from clinicians and patients. Here is a checklist of questions to ask before deciding on a vendor:
- Is the platform cloud-based?
- What equipment is included for vital and biometric monitoring?
- How does connectivity work?
- Does the solution offer video visit capabilities?
- What is the virtual visit platform?
- Is the software platform secure and HIPAA compliant?
- Can I use this to get reimbursed?
- Is a mobile application available?
- Do you offer technical support to patients and providers?
- How does logistics and inventory management work?
- Will I have access to a Client Success team? What does that relationship include?
- Do you offer marketing guidance and support?
- What is the total cost of ownership?
- Do you involve the patients’ caregiver in any way?
- Is the care plan customizable by patients?
Need help getting started with your telehealth program? Check out our 6 Essential Steps to Building a Scalable and Profitable Telehealth Program white paper
Solutions Overview
At Health Recovery Solutions (HRS), we offer comprehensive telehealth solutions across the care continuum. Whether you’re caring for recently discharged patients who are at high risk of readmission, patients who require intermittent follow-up visits, or patients who are looking for more connected care, HRS offers solutions for all.Telehealth Solutions for Every Patient: What HRS Offers
PatientConnect® Complete
What is it: A tablet and advanced biometric Bluetooth offering that allows patients to record their vitals at home while providers collect and monitor this biometric data in real-time and respond to potential issues as soon as they arise.
Suitable for: High-risk chronic disease patients recently discharged from the hospital or at risk of readmission. These patients require comprehensive monitoring tools to support ongoing management of their disease(s).
PatientConnect® Mobile
What is it: A Bring Your Own Device (BYOD) solution that enables patients to access the HRS patient engagement software from their personal smart device.
Suitable for: Any patient with an Android or iOS device who will benefit from on-demand communication, education tools, medication management, and more. This is more appealing for younger populations as a care transition solution and a lower cost option for patients who own a mobile device.
PatientConnect® Voice
What is it: An interactive voice response (IVR) calling service directly to the patient's phone that delivers reminders or customized messages to patients across the healthcare spectrum.
Suitable for: Any patient who would benefit from automated calling reminders and symptom surveys. This offering works as both a stand-alone feature and an augment to other HRS solutions.
PatientConnect® Core
What is it: A tablet-only solution that delivers on-demand connection between the patient and provider.
Suitable for: Any patient who would benefit from medication reminders and survey questionnaires but does not need extra biometric tracking peripherals in their daily care plan. This offering excels in hospice and palliative care.
Key Telehealth Features
To better understand how to shape your telehealth program, take a look at these key telehealth features so you can match them to your clinicians’ and patients’ needs.
Virtual visits and communication tools
Patients can communicate in real time with healthcare providers on a telehealth device, usually a tablet or a mobile phone, via video calls, phone calls, and in some instances, text messages. But with HRS solutions, it doesn’t end there.
The HRS telehealth platform provides 24/7 technical support and troubleshoots problems on both the patient’s and healthcare provider’s end. This could be anything from difficulties pairing Bluetooth devices to setting up the first virtual visit to loading educational materials onto the tablet.
With three-way calling, patients can have a consultation with more than one clinician or even have their caregiver on the call at the same time.
Throughout the years, we have established telehealth virtual visits best practices from our many implementations to help you have an engaging session with your patient. Here’s a quick guide to help you get started:
Basic Best Practices During a Telehealth Visit
- Make eye contact
- Ensure the patient can hear
- Reintroduce yourself
- Take your time
- Leave time for questions
- Find a private space
- Follow-up before the call
- Prepare for the call
Symptom surveys
Daily symptom surveys provide real-time insight into the patient’s symptoms, including symptoms relating to mental health or other comorbidities. Symptom surveys are essential for tracking condition status and recovery progress.
Used in conjunction with these other key telehealth features, symptom surveys can help paint a complete picture of the patient’s disease-state and their understanding of their condition.
This helps a clinician to deliver consistent patient-centric care as they have a better understanding of how their patients’ day-to-day state and behaviors change, not just how they’re feeling on the day of their appointment itself.
Medication reminders
Alerts and voice calls that inform when medications are overdue can be set up to promote medical adherence. A crucial aspect of recovery and treatment efficacy depends on medication adherence and for the most part, this responsibility lies with the patient.
Telehealth has been proven to assist with improving medication-taking behavior as healthcare providers can take a more proactive role in the process, while patients gain access to tools they need to keep track and record their medication schedule.
Educational modules
Education can be easily delivered throughout a patient’s episode of care via teach-back quizzes and informational videos tailored to each patient’s diagnosis, treatment, or medication. The completed modules can be reviewed at any time by accessing the telehealth software.
Condition-specific education helps the patient understand their conditions and the actions they can take independently to alleviate their symptoms. It helps them understand the importance of engaging with the telehealth program and provides them with actionable insights into their condition, ultimately helping to improve health literacy and overall engagement in their health.
These are just some examples of how you can incorporate patient education into your telehealth program:
- Disease prevention across patient populations and disease-management groups.
- CDC and other official public resources.
- Building knowledge of conditions and decreasing complications by virtual teaching techniques, clinical guidance, continuous monitoring, and connectivity.
- The capability to electronically upload agency-specific or proprietary resource materials important to your organization or patient’s condition (for example, zone tools, exercise guidelines, dietary instructions, educational plan of care, pamphlets, etc.).
- Recorded training sessions to upload to your organization’s online educational platform.
Wound imaging
Wound care imaging as a telehealth feature works by enabling the patient to take photos of their wound recovery progress and send them to a wound care specialist. It allows clinicians to evaluate patients’ wounds anytime, anywhere and respond quicker in case there are complications.
Patients, caregivers, and clinicians can coordinate with wound care specialists through telehealth and remote patient monitoring platforms, working together to understand necessary changes to patient care and prevent hospitalizations.
Caregiver application
The HRS platform also incorporates the caregiver into the patient’s care plan with the CaregiverConnect mobile application. Caregivers can communicate with the patient using the application, and patients can reach their caregiver directly through their device.
With the free CaregiverConnect application, the caregiver can help monitor and track the patient’s daily progress. They will have full access to the health information tracked like vital signs, symptom survey responses, and clinical team communication through video, voice, and text messaging.
Bluetooth monitoring (remote patient monitoring devices)
Remote patient monitoring devices or RPM devices are non-invasive devices that acquire patient data so providers can understand and track patient symptoms. These typically feature Bluetooth connectivity and transmit health data to the telehealth device where it is processed and then stored on the platform.
There are many types of remote patient monitoring devices that you can use with your telehealth program. What you decide on depends on your patient’s needs and their adeptness at using the device on their own.
- Blood pressure cuff
- Pulse oximeter
- Weighing scale
- Thermometer
- Glucometer
- Spirometer
- Wearables like the BioSticker or activity trackers like FitBit or Apple Watch
- ECG + stethoscope
EMR integrations
A telehealth software that’s integrated with your EMR will communicate with one another through a bidirectional workflow, which essentially means both platforms can send and receive data. This integration is crucial as it increases efficiency and improves care quality, empowering healthcare providers to make informed decisions, facilitating faster diagnosing, lowering prescribing errors, and subsequently, improving patient outcomes.
EMR integration bridges the gap between telehealth and patient data and minimizes duplication of records and processes. As a result, there is a single, updated source of truth for all patient data.
Clinical dashboard—the provider experience
On the clinician’s end, telehealth provides a dashboard for monitoring patients and all the information gathered via remote patient monitoring, symptom surveys, virtual visits, wound imaging, and more.
This enables providers to monitor, triage, and care for their patients in real time. Here’s a guide on triaging risk alerts on a telehealth platform to help you leverage the benefits of the clinical dashboard:
- Verify and validate the reading with the patient or caregiver.
- Confirm accurate medication regimen was followed on that day and previous days.
- Check for abnormal symptoms.
- Perform a visual assessment.
- Escalate to the necessary intervention, if necessary.
- Document the intervention.
Benefits of Telehealth
The advantages of telehealth for your healthcare organization are immense and improving patient outcomes and reducing cost of care are just a few of them. To answer the question why is telehealth important in today’s healthcare setting, take a look at the following benefits.
Medication Adherence
Telehealth is a proven way to improve medication adherence as patients can get alerts when it is time to take their medication. If a dose is missed, that information is recorded and available for the clinician to review. Patients can also get reminders for when their prescription is due for refill so the entire process becomes more seamless and engaging.
Patient Engagement
A patient who is engaged with digital patient engagement tools are able to complete daily tasks related to their medical care at their own pace. They understand the importance of these tools, how to use them, and the positive impact it has to their health outcomes.
Patient Satisfaction
Telehealth solutions can help improve patient experience and satisfaction in a value-based care ecosystem, and give you a boost in your Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS) score. It helps you meet your patients’ needs, like feeling connected and engaged with their clinician, receiving the information they need to manage their condition, and having access to a platform that makes care more convenient. All of this leads to higher overall patient satisfaction.
Cost of Care
The cost savings as a result of telehealth implementation can be seen across departments and functions. It makes an immediate impact in reducing travel expenses for doctors and nurses when you switch from physical follow-up visits to virtual visits. In the long term, telehealth increases the productivity of your team, automating costly manual processes and helping your medical staff focus their time on high-value tasks.
Continuity Across Continuum
A comprehensive telehealth platform ensures continuity of care for your patients. Transition care doctors or nurses can make use of video call and chat functions to communicate and stay connected with patients. This cuts down the time and costs associated with in-person visits, and also minimizes transfer-associated risks.
Provider/Patient Communication
Virtual visits are not under the same constraints as physical check-ins and thus provide a more convenient method of communication between providers and patients. Besides video calls, both the provider and patient can also reach out to each other via voice calls or text messages.
Caregiver Involvement
Telehealth platforms provide caregivers with patient information and an additional channel for communication and monitoring. For example: caregivers can monitor patient vitals including access to view patient adherence for each metric, as well as video and chat functionality. Keeping caregivers informed and connected with their loved ones takes away the burden of worrying and having to physically check up on them.
Access to Care
Telehealth is able to reduce disparities in access to care because it provides patients convenient access to specialists in situations where physically going to a hospital is difficult. This is particularly advantageous for healthcare services in rural areas and palliative care where healthcare providers can now meet their patients where they are.
Reduced Readmission
Healthcare providers can select an automated care plan and tailor that based on the patient’s needs and medication schedule. Through high-risk monitoring and customized risk alerts, clinicians can respond quickly at the first signs of distress, avoiding costly readmissions and preventable emergency department visits.
Reduced Isolation and Loneliness
Telehealth services provide a way for patients to feel connected to their healthcare provider, caregiver, or family members. This reduces negative outcomes resulting from feelings of loneliness and isolation, especially in the midst of a pandemic.
Telehealth Use Cases for Specific Conditions and Program Types
Chronic Disease Management
Telehealth provides access to populations with chronic diseases to tools that improve their health status and strengthen their self-management skills. It’s effective in managing conditions like chronic obstructive pulmonary disease (COPD), congestive heart failure (CHF), diabetes, hypertension, and more.
Use case:
A patient with acute cardiovascular disease (CVD) can communicate with their clinician through video and voice calling in real time to monitor heart rhythm, breathing patterns, blood pressure, edema, and more. Clinicians can make necessary adjustments to the patient’s medication, exercise, or diet routine and encourage control and confidence in their health. Catching symptoms or vital changes early can help avoid exacerbations and save a life.
Post-surgical and Physical Therapy
Patients can stay connected with their physical therapists beyond in-person visits. They’re able to engage with physical therapy sessions from the comfort of home, reducing the need to travel especially when they’re in recovery.
Use case:
A patient recovering from Total Joint Replacement (TJR) surgery can monitor their daily vitals with biometric Bluetooth devices that record blood pressure levels, heart rate, and oxygen saturation levels. Additionally, they can answer symptom surveys to communicate their physical condition as well as pain scores to the provider, ensuring prompt and appropriate follow-up action should certain readings trigger a risk alert.

Oncology
Providing telehealth solutions for individuals with cancer helps them regain a sense of normalcy especially when their daily life is consumed by cancer treatments. By extending cancer care to the home, oncology patients can decrease the amount of stress and time they spend in hospitals, which then lowers their risk for catching infectious diseases.
Use case:
A patient undergoing chemotherapy can be enrolled into a telehealth program and sent a daily survey to report on 12 of the most common symptoms associated with their condition. Any significant changes will trigger a risk alert to the nurse or physician and they can take action like remote symptom management, prescribing supportive medications, active chemotherapy dose modifications, and specialty referrals.

Prenatal
Telehealth for the expectant mother, when built around a family-centric model, embraces the emotional element of pregnancy while also meeting important goals of prenatal care like detection, management, and amelioration of complications when they arise.
Use case:
A pregnant woman is able to monitor her weight and track both her blood pressure and fetal heart rate in the comfort of her own home. If a patient experiences abnormal or confusing results, she simply reaches out to her clinician via video call, voice call, or text messaging.

Postpartum
New mothers can better navigate the postpartum stage, which can be a challenging time, with the help of telehealth. Telehealth and remote patient monitoring tools enable new mothers to receive care conveniently from their home.
Use case:
The new mother has access to symptom surveys and educational videos within the telehealth device, as well as direct access to her clinician or nurse. This real-time connectivity allows the new mother to get guidance on postnatal care for mother and baby like diet, physical activity, breastfeeding, sleep, and more.

Primary Care
By leveraging telehealth, hospitals can better utilize bed capacity and focus on treating COVID patients within the hospital walls while also maintaining connection with their primary care patients without traditional office visits.
Use case:
As utilization nears maximum capacity for hospitals bearing the brunt of COVID-19, healthcare providers can leverage telehealth to channel some of their primary care services virtually, freeing up their clinicians and nurses to focus on treating inpatients. At the same time, patients receiving primary care get peace of mind knowing that they are still connected to their provider from the safety and convenience of their own home.

Hospital at Home
Hospital at home programs have benefited primarily those with non-COVID-19 conditions. However, for some patients with COVID-19 (those that are lower risk and/or stable), the hospital at home model can enable patients to leave the hospital earlier than otherwise would have been possible without a technology option to support them during their recovery.
Use case:
The program begins by identifying patients who can safely return home from the emergency department instead of being admitted. The patient is transported to their home via ambulance and receives home-based care specific for their condition, like blood tests, X-rays, and medication infusions. They may receive visits from medical staff as part of the procedure if needed and their daily vitals are recorded via remote patient monitoring devices.

Pediatrics
Pediatric telehealth could potentially help with improving patient and family satisfaction, saving costs, and reducing emergency room visits. For working parents, keeping their children healthy means missing work less often, which is an added benefit.
Use case:
Parents can enroll their children in a telehealth program to monitor for asthma. They could use any number of remote patient monitoring devices like Bluetooth spirometers, smart inhalers, wearables, or pulse oximeters to optimize asthma management. Paired with symptom surveys and virtual visits, this gives both parents and providers a better way to manage the patient’s asthma conditions and take action before it worsens.

Behavioral Health
Virtual visits and direct messaging enable clinicians to provide behavioral health services to patients through an intuitive platform, from a remote location. Patients have access to effective, high-quality mental healthcare wherever they may be, even in rural locations.
Use case:
A patient with comorbid depression resulting from chronic illnesses can be put on a telehealth program that includes daily telemonitoring of vitals, symptoms, and medication intake, on top of weekly virtual therapy sessions. The telehealth nurse also communicates with the patient’s primary care physician to coordinate their antidepressant prescription.

Alzheimer’s
For the Alzheimer’s patient, especially in the early stages of the disease, telehealth can provide a solution to the difficult problem of traveling. With the use of telehealth, the patient can be seen by a specialist who may be hundreds of miles away without the need to travel the distance to the clinician’s office.
Use case:
Telehealth helps an Alzheimer’s patient stay at home, prioritizing “aging in place.” The patient can remain at home while receiving care, ensuring continuity of the care environment and avoiding stressors that may trigger reactions such as anxiety, confusion, and agitation. This also promotes patient safety within the home when used with features like wandering prevention tracking, action triggered lighting, and video monitoring.

Member Management
Telehealth supports care coordination—it helps the provider team stay connected with the member post-discharge. The exchange of clinical information in real time makes telehealth a vital tool to facilitate continuous communication between the member and their post-acute provider.
Use case:
From the minute they are discharged from the hospital, the clinician can keep track of the member through the transitionary period and into the recovery stage, so care does not end at the hospital door. In between clinic visits, patient education and teach back quizzes serve as a touch point that helps members understand and manage their health for better outcomes.

Palliative Care/Hospice
For palliative patients, care coordination, patient education, and symptom and medication management are critical to improving quality of life and preventing adverse health events. Telehealth services can offer patients and their families the advanced care necessary to ensure their needs are met.
Use case:
The palliative interdisciplinary team can remain involved throughout a patient’s palliative care plan, looping in the caregiver and specialists as needed. Virtual visits remove the burden of traveling and the patient can receive quality care at home.

Reimbursement and billing
With remote patient monitoring now included in the Centers for Medicare and Medicaid Services’ (CMS) reimbursement policies, here are five primary RPM codes to take note of:
| 99091 | Can be billed $59 once per 30-day period for a minimum of 30 minutes of review data only by physicians or qualified health care professionals. |
| 99091 | Covers the set up and patient education on RPM equipment including initial setup of devices, training and education, and any services needed to enroll the patient on-site ($21). |
| 99454 | Covers remote monitoring of physiological data with a device; reimbursement of $69 can be filed once every 30 days. |
| 99457 | Provides a $54 reimbursement each calendar month for a minimum of 20 minutes of live communication with the patients by physicians, qualified health care professionals, or clinical staff. |
| 99458 | An add-on for CPT code 99457 and cannot be billed as a standalone code; it is used for each additional 20 minutes of remote monitoring (allows for $43 in billing per calendar month). |
Future of Telehealth
The telehealth trend has been on the rise even before COVID-19 days. Since the pandemic, however, the demand for telehealth technology has surged and accelerated its adoption as an integral part of healthcare worldwide.
It’s not sufficient to just implement telehealth—leading healthcare organizations are looking at strategies to ensure their telehealth programs are not only successful, but future-proof.
To get there, one of the things to address is data interoperability. As more and more healthcare data becomes readily available through the power of connected devices, telehealth platforms, and healthcare software, it’s mission-critical to ensure all this information can flow across systems and are easily extracted. The potential here is immense and the more complete the electronic medical record is, the better healthcare providers are able to make decisions for improved patient outcomes.
Another important factor is the power of artificial intelligence combined with predictive analytics. Once the healthcare data foundation has been built, providers can apply machine learning algorithms to this data and get insights into the most effective and efficient treatments and interventions that will bring about optimal results. Being able to apply predictive analytics to areas like ED utilization and patient risk factors can help healthcare providers manage their resources efficiently, gain cost savings, and deliver quality care.
Hear from Doug Lang, HRS' Vice President of Client Growth about the future of telehealth below:

Ready to get started on your telehealth program? See how our comprehensive solutions fit in with your healthcare goals.
Download the 6 Essential Steps to Building a Scalable and Profitable Telehealth Program White Paper
In this white paper, learn about:
- Establishing goals
- Determining your financial plan
- Choosing a technology partner
- Building clinician and patient buy-in
- Other essential factors to consider to ensure your program is successful



