As healthcare shifts towards value-based care, payors need to adapt to meet their member's needs. Remote patient monitoring (RPM) and telehealth are tools that are beneficial for payors as they help proactively manage their members across the care continuum and acuity spectrum. In this blog post, we will discuss the six reasons why telehealth makes sense for payors.

1. Improvements in HEDIS measures, star ratings, and member retention
Health plans are measured against HEDIS and star ratings to evaluate the effectiveness of care delivery, which is used as a benchmark for how a health plan manages care for its members. RPM and telehealth enable payors to better manage complex chronic conditions, deliver preventive services, and provide high-quality, personalized service to members. This combination yields positive member experiences, which improves satisfaction scores and ultimately star ratings. By offering personalized care, convenient access to specialists, and communication tools for seamless care coordination, member satisfaction improves, resulting in increased member retention.
2. Achieve more efficient utilization and care management
Every member's healthcare journey is unique, and payors are looking to understand each member's longitudinal care journey before an acute care episode or the exacerbation of a condition. RPM and telehealth helps payors to give members transparency into their condition and care plan, promote medication compliance and health literacy, and seamlessly integrate the support of a caregiver. By offering personalized care, convenient access to specialists, and communication tools for seamless care coordination, member satisfaction improves, resulting in increased member retention.
3. Optimize care coordination between payor and provider
It is critically important to address members' health concerns at the first point of presentation. RPM and telehealth enable payors to triage member populations in more effective ways, coordinate better with providers, and curb unnecessary costs. RPM has the potential to support successful transitions between inpatient and ambulatory episodes and provide a more continuous cycle of healthcare for members with chronic conditions. RPM and telehealth can serve to delegate tasks from overstretched providers to care coordinators, supporting both providers and members.
4. Enhance efficiency in care delivery through automation tools
Digital innovations have paved the way for a more seamless care experience between members and their providers. RPM and telehealth provide physicians and payors with risk stratification information, risk alerts tied to populations, and ways to modify utilization, introducing new efficiencies in care delivery. Pairing real-time data and insights with targeted interventions allows plans to reduce unnecessary costs, manage inappropriate utilization, and, ultimately, deliver better health and quality outcomes.
5. Avoid delays in treatment and increase access to care
Access to appropriate transportation, available specialists in their location, and long wait times for in-person appointments with the provider they need access to are a few reasons why members delay participating in in-person appointments that support their healthcare management. RPM and telehealth enable payors to provide virtual care to their members, which reduces delays in treatment and increases access to care.
5. See a decrease in costs by shifting in-person care to remote care
RPM and telehealth help to shift in-person care to remote care, which leads to a decrease in costs. By providing virtual care, members can receive the care they need without traveling to a healthcare facility, which reduces transportation costs. Additionally, by using RPM and telehealth, payors can identify potential health problems early, which reduces the cost of treating the condition in the future.
Partnering with HRS
HRS payor partners are implementing telehealth and remote monitoring to manage member outcomes across all populations. When you work with us, you get proven solutions that enable comprehensive, value-based care.
Remote Patient Monitoring: A Comprehensive Solution
In conclusion, telehealth and remote patient monitoring provide payors with a comprehensive solution to improve care delivery, reduce costs, and enhance member satisfaction. The implementation of these tools can optimize care coordination, increase efficiency, and provide timely access to care while improving the quality of care delivered.
Payors that embrace telehealth and remote patient monitoring can effectively manage their members across the care continuum and acuity spectrum, resulting in positive health outcomes and a healthier bottom line. As the healthcare industry continues to shift towards value-based care, payors who invest in telehealth and remote patient monitoring will be well-positioned to meet the changing needs of their members and succeed in the evolving healthcare landscape.
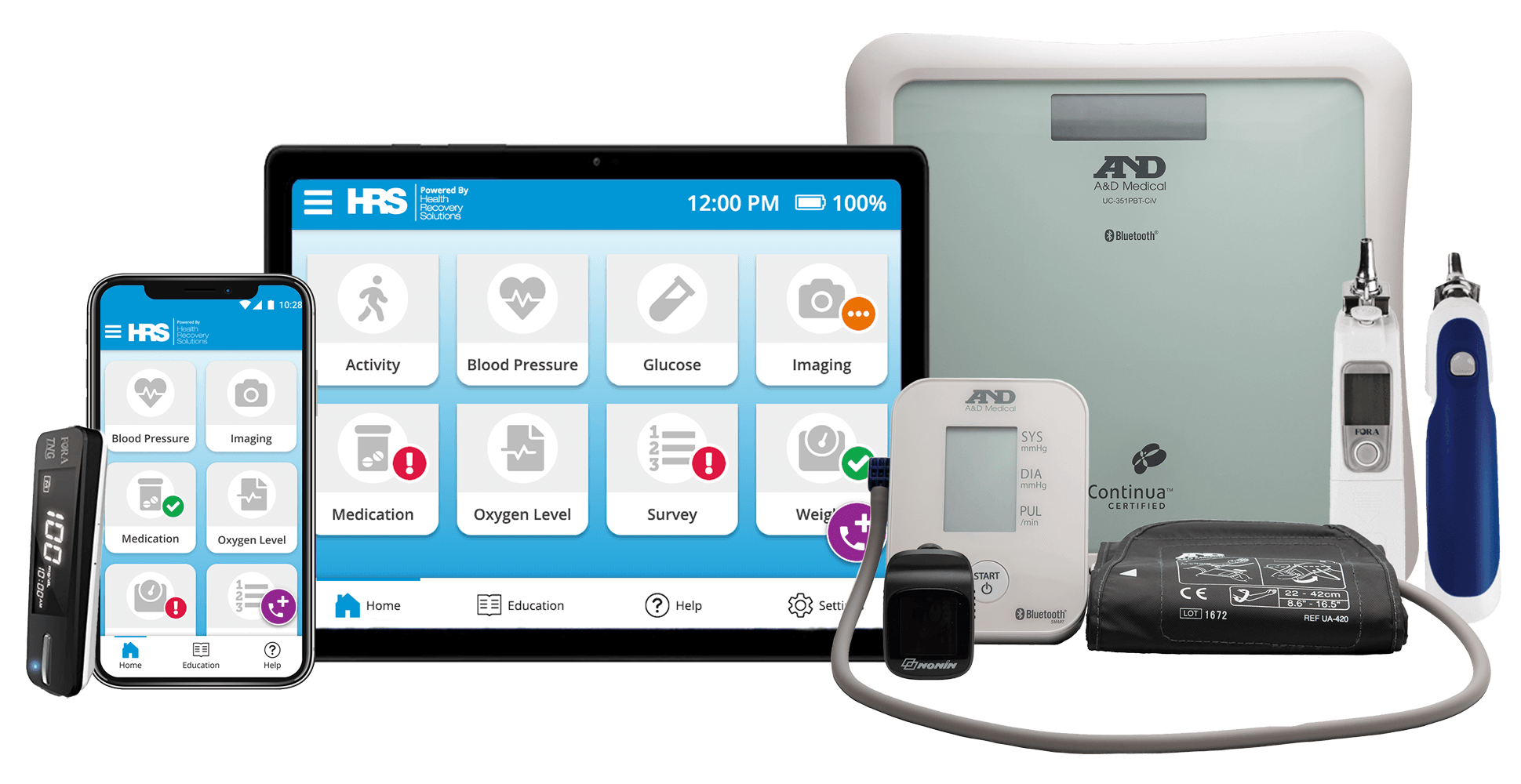
Connect with an HRS Digital Health Advocate
Learn about our comprehensive suite of telehealth and remote patient monitoring solutions during a personalized demonstration.
