Many of the issues facing the healthcare industry in 2023—including soaring expenses, clinician shortages, and a changing regulatory landscape—are expected to remain challenges in 2024. C-suite leaders are making tough decisions in an effort to serve their communities more efficiently and equitably while maintaining a healthier bottom line.
As traditional healthcare models undergo change, adoption of remote patient monitoring (RPM) is still very strong. The global RPM market, estimated at $14 billion in 2023, is expected to increase at a rate of 20.1% annually and reach $41.7 billion by 2028. Growth is being driven by multiple factors:
- Continued expansion of hospital at home and post-operative care programs
- Need for more cost-effective services
- Increasing geriatric population
- Rising prevalence of chronic conditions
- Emphasis on patient-centered care
- Focus on underserved patient populations
Let’s look at eight trends that we think could impact the RPM landscape in 2024.
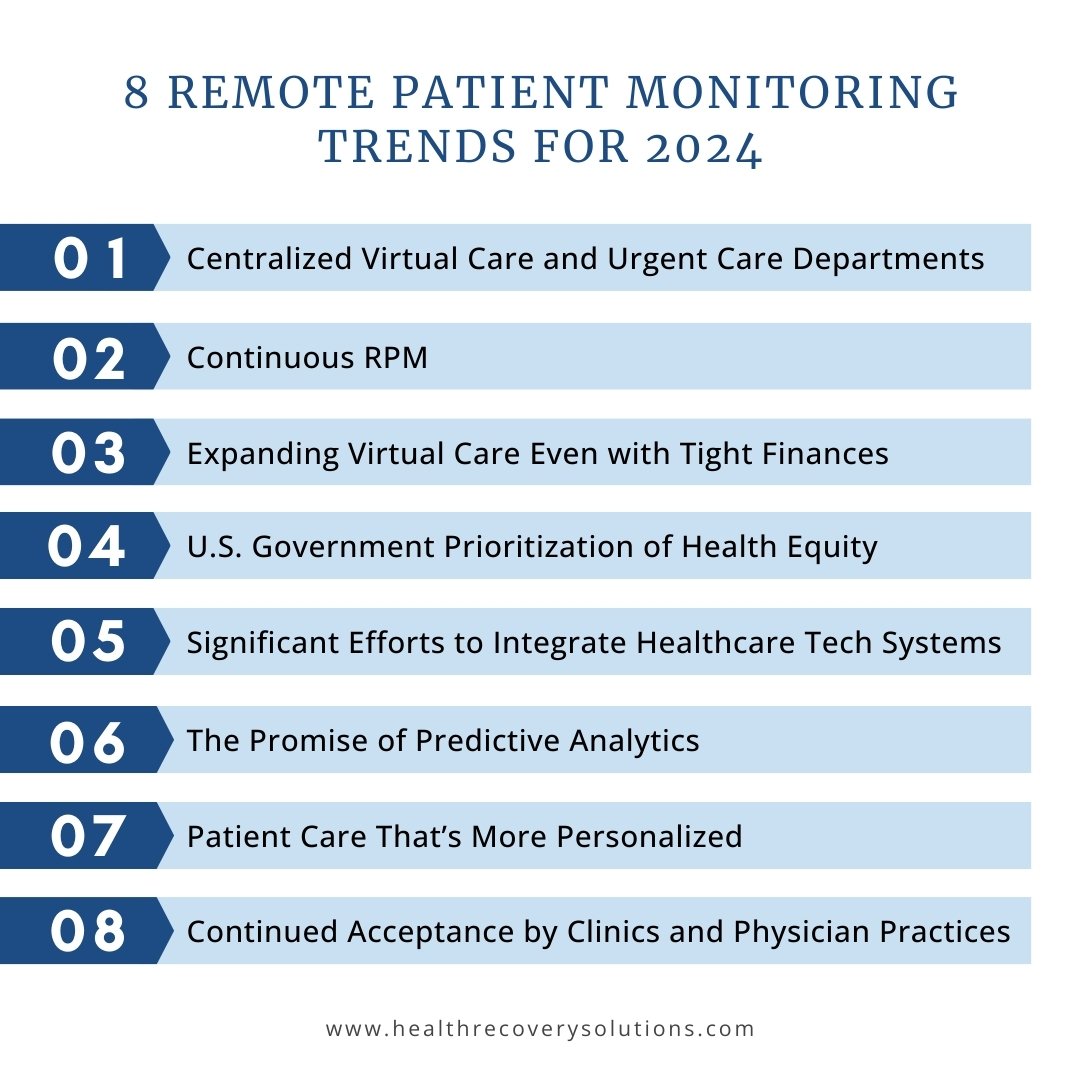
1. Centralized Virtual Care and Urgent Care Departments
The pandemic revealed the efficiency and effectiveness of telehealth to the world. Now, virtual healthcare is moving well beyond telehealth doctor visits and routine patient monitoring. Leading providers like Lee Health have created remote patient management programs—using tools to go beyond monitoring into the active management of outpatient problems through a centralized virtual care department. Providers are also setting up virtual urgent care departments, with face-to-face exams and medical visits available 24 hours a day, seven days a week. Given the proven results and reasonable costs of RPM, we expect new ways to use the technology to emerge going forward.

Lee Health: Transforming Remote Patient Monitoring into Remote Patient Management
See how Lee Health, the 4th largest public health system in the U.S., transformed care delivery and learn about the next phase of their evolution: pushing the boundaries of virtual care.
2. Continuous RPM
Most RPM technology in operation today measures patient vitals at certain times of the day. To fill a need identified by providers, a pilot program is now exploring the benefits of performing continuous metrics for body temperature, heart rate, respiratory rate, pulse oximetry, and ECG. This can be especially useful for high acuity patients in cardiac care or hospital at home programs. We’ll share the results of this industry-leading pilot program as they become available but it's safe to say that continuous remote monitoring will continue to be a part of the RPM conversation in 2024 and beyond.
3. Expanding Virtual Care Even with Tight Finances
Low margins and high expenses are top-of-mind issues for healthcare financial leaders. Many healthcare systems are looking to transition to new operating models that can deliver quality outcomes at a lower cost by consolidating less profitable service lines and cutting unnecessary spending.
Even as traditional services like inpatient care are scaled back, those that have proven to be cost-effective — including virtual care, RPM, and hospital at home —continue to expand. Healthcare leaders know that these technologies have been proven to reduce unnecessary emergency department visits, increase bed capacity during hospital surges, improve clinical decision making, and reduce the burden on the healthcare system.
4. U.S. Government Prioritization of Health Equity
Providing quality healthcare for everyone will remain a top priority for government healthcare leaders in 2024. The Centers for Medicaid and Medicaid Services (CMS) released an updated framework for health equity, and the Joint Commission is holding providers to high standards and offering advanced certification in this area.
Grant money is also flowing to Federally Qualified Health Centers (FQHCs), which have become an important health safety net by providing care to underserved areas or populations in the U.S. These outpatient clinics qualify for specific reimbursement systems under Medicare and Medicaid.
Because they’re located in sparely populated areas with a shortage of healthcare providers, FQHCs are a natural fit for RPM technology, allowing professionals to efficiently monitor and stay in touch with patients. The good news is that CMS released its final rule for Medicare payments under the Physician Fee Schedule (PFS) in 2024, allowing for FQHCs and RHCs to bill for RPM services under the general management code G0511. This change takes effect on January 1, 2024, empowering FQHCs to expand access to remote care and further increase health equity.
This is another example of how trends in reimbursements and Current Procedural Terminology (CPT®) codes are helping to drive RPM expansion.
5. Significant Efforts to Integrate Healthcare Technology Systems
For years, healthcare systems and providers have operated in silos, with little sharing of data. Most electronic health records (EHRs), medical devices, and information technology systems simply don’t communicate with one another. As a result, clinical caregivers often lack a holistic patient view as they diagnose and treat their patients, and administrators don’t have the data they need to make informed decisions about the populations they serve.
All of that is changing, thanks in part to a major push to adopt the 21st Century Cures Act by the Office of the National Coordinator for Health Information Technology (ONC). The act is designed to support seamless and secure access, exchange, and use of electronic health information, providing benefits to both health care providers and patients.
RPM should be a key part of this more open and integrated healthcare ecosystem, providing vital electronic data that caregivers can use to monitor progress, make more accurate treatment decisions, and ultimately improve outcomes.
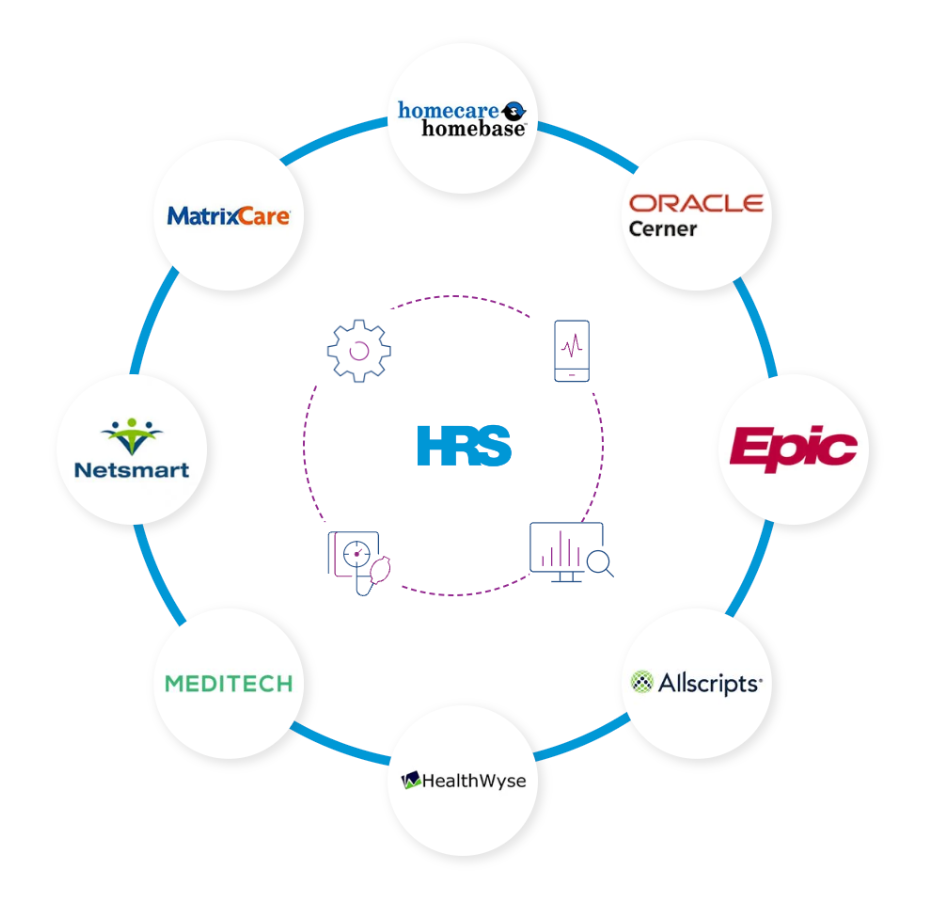
EHR Integration Support
Simplify the process of integrating new healthcare technology into your tech stack. The HRS Integrations Team supports all technical aspects, QA testing, and troubleshooting to integrate the HRS ClinicianConnect® portal with your EHR.
6. The Promise of Predictive Analytics
Talk of new artificial intelligence (AI) technology and applications is everywhere—especially generative AI, which can learn and adapt based on the data it receives. Many exciting new uses for AI are in the works, including healthcare virtual assistants (HVAs) that can help patients take greater control of their care and get the information and support they need 24/7.
Advancements in AI and machine learning (ML) are also expanding our capabilities when it comes to predictive analytics. Leveraging predictive analytics, healthcare technology providers can use historical health data to identify patterns and trends that can accurately forecast health outcomes.
This can create powerful possibilities for RPM programs, which collect real-time data on changes and trends in a patient's condition over weeks, months, or even years. By applying predictive analytics to this vast trove of data, healthcare providers can tailor personalized care plans to meet each patient’s specific needs. Providers can also develop more targeted treatments for larger groups of patients who share similar characteristics.
7. Patient Care That’s More Personalized
With patients taking greater control over their healthcare, it’s no wonder that they have strong opinions about the way they communicate with providers and their chosen medical devices.
According to one survey, 55% of patients said they would think about changing providers if their communication preferences weren’t met. In the same survey, 81% of patients said their communication preferences had changed since the pandemic began.
This shift in expectations from patients as consumers of healthcare coincides with new opportunities to leverage big data, ML/AI, and predictive analytics to provide a more personalized experience for each individual. As the technology evolves, data, trends, and insights can be personalized and self-reflected back to the patient to assist in guiding and managing their own wellness, encouraging and empowering them to play a bigger role in their own care.
8. Continued Acceptance by Specialty Clinics and Physician Practices
Growth in RPM Medicare reimbursements has increased the use of the technology among specialty clinics and physician practices. RPM is a proven way for caregivers to establish a close connection with patients who require ongoing management and monitoring. The ease of implementation and convenience of RPM systems can improve patient satisfaction, boost patient adherence, and close gaps in care. In addition, RPM can be quickly adapted to fit a wide variety of medical specialties.
This trend aligns closely with the broader movements toward patient-centric care and concierge medicine.
The Future of RPM: Technology, Services, and Growth
From new technology to expanded services to reimbursement changes, exciting things are happening in the RPM industry. As providers continue to focus on cost-effective services that improve care, boost efficiency, and increase patient convenience, RPM should play an ever-larger role in the healthcare industry in the coming years.

Remote Patient Monitoring & Care Management Solutions
Partner with the only single-source provider in remote care with a proven track record of success. Achieve better clinical outcomes and ROI by leveraging HRS' best-in-class clinical expertise, logistics, analysis, and the industry's leading, most advanced remote care technology.