A Comprehensive Guide to Health Equity in the U.S.
Health equity is a fundamental principle of public health that aims to ensure that everyone has an equal opportunity to achieve optimal health.
Unfortunately, disparities in health outcomes persist in the United States and around the world. Achieving health equity requires understanding the concept of health equity, recognizing the current state of health inequity, identifying the barriers that contribute to these disparities, and implementing strategies to address them.
“Looking back over the last century, as a health industry we’ve made great gains. Whether it's antibiotic therapy or vaccines, reducing the spread of infections and diseases that impeded the quality or length of life. But, unfortunately, a lot of these gains have not been experienced across different populations. We continue to see a lot of issues that should be behind us and it's really important for us to ensure that as we build our clinical programs, as we build technology, that it has health equity as a central and core piece.”

Understanding Health Equity
What is Health Equity?
The Centers for Medicare & Medicaid Services (CMS) defines health equity as: the attainment of the highest level of health for all people, where everyone has a fair and just opportunity to attain their optimal health regardless of race, ethnicity, disability, sexual orientation, gender identity, socioeconomic status, geography, preferred language, or other circumstances.
Generally speaking, health equity is the absence of systematic disparities in health between social groups who have different levels of advantages or disadvantages. It goes beyond the concept of equality, which seeks to provide everyone with the same resources or opportunities. Health equity recognizes that certain individuals and communities may require additional support to overcome the unique challenges they face in achieving optimal health.
Health equity also acknowledges the impact of social determinants of health, which are the conditions in which people are born, grow, live, work, and age. These determinants, such as income, education, employment, and social support, significantly influence an individual's health status.
Why is Health Equity Important?
By promoting health equity, we can reduce disparities in health outcomes such as mortality rates, disease prevalence, and access to healthcare. Advancing health equity is a way to improve the overall health and well-being of entire populations.
By addressing the root causes of health disparities and providing targeted interventions, we can prevent chronic diseases and reduce healthcare utilization.

Health Equity
Health equity is the absence of systematic disparities in health between social groups who have different levels of advantages or disadvantages.
Health Equity in the United States
The United States, despite being one of the wealthiest nations in the world, faces significant health inequities. Certain populations, including racial and ethnic minorities, low-income individuals, and rural communities, experience higher rates of chronic diseases, limited access to quality healthcare, and poorer health outcomes compared to more privileged groups.
These disparities can be attributed to a complex interplay of socioeconomic factors, systemic racism, and other social determinants of health.
An analysis by KFF of the health outcomes for racially-diverse populations found that racial and ethnic minorities struggle with:
Chronic Disease Burden
Financial Challenges
Maternal Health
Growing Population
These disparities are not solely due to genetic factors but are largely influenced by social determinants of health, including limited access to healthy food options, safe neighborhoods for physical activity, and quality healthcare services.
Income inequality also drives health inequity. Low-income individuals also face unique challenges in accessing healthcare. Limited financial resources often result in delayed or inadequate medical care, leading to poorer health outcomes. Additionally, the lack of health insurance coverage among low-income populations further exacerbates health inequities, as preventive care and early interventions are often unaffordable.
Language is another factor that impacts access to care. For patients with Limited English Proficiency (LEP), finding care, booking appointments, and communicating with physicians at visits can all be significant challenges.
On a similar note, health literacy, or the degree to which individuals have the capacity to obtain, process, and understand basic health information and services needed to make appropriate health decisions, impacts health equity. When literacy is limited, patients may not be able to understand their care options, manage conditions, or make decisions around their care.
Just as limited health literacy can hinder individuals' ability to navigate the healthcare system and make informed decisions about their care, so too do geographical barriers. According to the CDC, 46 million+ people, or 15% of the total population, live in rural areas and they are more likely to die from heart disease, cancer, and stroke. In rural communities, deaths from unintentional injury are also 50% higher than urban areas. Limited access to healthcare facilities, long travel distances, and a shortage of healthcare professionals make it difficult for individuals living in rural areas to receive timely and quality care.
In this brief, 1-minute video clip, hear Sudeep Pisipaty, HRS' Head of Commercial Strategy & VP, Strategy – Value Based Care, discuss the intersection of social determinants of health and the patient journey in healthcare.
Addressing health inequities in the United States requires a comprehensive approach that addresses the underlying social determinants of health. This includes improving access to affordable healthcare, implementing policies that promote health equity, and addressing systemic racism and discrimination within the healthcare system. Fortunately, advancing health equity is a key priority for organizations like CMS and the Joint Commission, which wield significant influence over the entire healthcare system.

The Key Benefits of Telehealth in Rural Areas
The healthcare industry has experienced a boom in telehealth and remote patient monitoring (RPM) programs in recent years. In this blog, we explore some of the key benefits of telehealth in rural areas and common challenges to expanding access to care.
CMS Framework for Health Equity (2022-2032)
The Centers for Medicare & Medicaid Services (CMS) is the largest health insurer in the United States - overseeing the Medicare, Medicaid, and the Children’s Health Insurance Program (CHIP) programs which provide care for more than 135 million Americans or 40% of the total population. By making health equity a key priority, CMS can have a significant impact on advancing health equity initiatives and closing the care gap for millions of Americans.
In 2022, the CMS established its Framework for Health Equity which is an integrated, action-oriented approach to advance health equity among communities who have been historically underserved or disadvantaged. It represents an update to the 2015 Medicare-focused CMS Equity Plan for Improving Quality in Medicare and outlines a 10-year plan to address five priority areas.
Five Priority Areas:
- Expand the Collection, Reporting, and Analysis of Standardized Data
- Assess Causes of Disparities Within CMS Programs and Address Inequities in Policies and Operations to Close Gaps
- Build Capacity of Healthcare Organizations and the Workforce to Reduce Health and Healthcare Disparities
- Advance Language Access, Health Literacy, and the Provision of Culturally Tailored Services
- Increase All Forms of Accessibility to Healthcare Services and Coverage
To address the first priority area, CMS released a new report in November 2022, The Path Forward: Improving Data to Advance Health Equity Solutions (PDF). The report outlines the current state of health equity data collection, details progress to date in improving data collection, and defines future actions to continue to improve health equity data.
The CMS Advancing All-Payer Health Equity Approaches and Development Model (AHEAD Model)
More recently, CMS unveiled a voluntary model designed to help states redesign healthcare delivery to improve the total population health of a participating state or region by improving the quality and efficacy of care delivery, reducing health disparities, and improving health outcomes.
Key Features of the AHEAD Model
- Primary Care: Focus resources and investment on primary care services, giving primary care practices the ability to improve care management and better address chronic disease, behavioral health, and other conditions
- Financial Incentives: Provide hospitals with a prospective payment stream via hospital global budgets, while including incentives to improve beneficiaries’ population health and equity outcomes
- Care Coordination: Address healthcare disparities through stronger coordination across healthcare providers, payers, and community organizations in participating states or regions
- Community Resources: Address the needs of individuals with Medicare and/or Medicaid by increased screening and referrals to community resources like housing and transportation
Joint Commission Health Equity Standards
Another organization advancing health equity is the Joint Commission (TJC). The TJC is a not-for-profit organization that accredits and certifies more than 22,000 healthcare organizations and programs in the United States.
Effective January 1, 2023, new and revised requirements to reduce health care disparities apply to organizations in the Joint Commission-accredited ambulatory health care, behavioral health care and human services, critical access hospital, and hospital programs.
6 Elements of Performance (EPs) for Healthcare Organizations:
- Designate an individual(s) to lead activities to reduce health care disparities
- Assess the patient’s health-related social needs and provide information about community resources and support services
- Identify health care disparities in the patient population by stratifying quality and safety data using sociodemographic characteristics
- Develop a written action plan that describes how to address at least one of the health care disparities identified in the patient population
- Take action when the goal(s) in the action plan are not achieved or sustained
- At least annually, inform key stakeholders (leaders, licensed practitioners, and staff) about progress to reduce identified health care disparities

Advancing Health Equity within Hypertensive & Postpartum Patient Populations Using RPM
This webinar, featuring Evara Health, discusses the latest best practices for improving health equity within chronic care (Hypertension, Diabetes) and maternal health (Prenatal/Postpartum) patient populations, focusing on social determinants of health and strategies for advancing equity using RPM & telehealth.
The Role of Healthcare Providers in Promoting Health Equity
Healthcare providers play a vital role in promoting health equity. To comply with the new standards from CMS and the Joint Commission, providers will need to take meaningful steps to advance health equity in their communities.
This can include:
Interpreters
Community Resources
Diversity & Inclusion Training
Establishing diversity and inclusion training programs within healthcare organizations to ensure that healthcare providers are knowledgeable and sensitive to the diverse needs of their patients
Patient-Centered Care
Telehealth and Health Equity
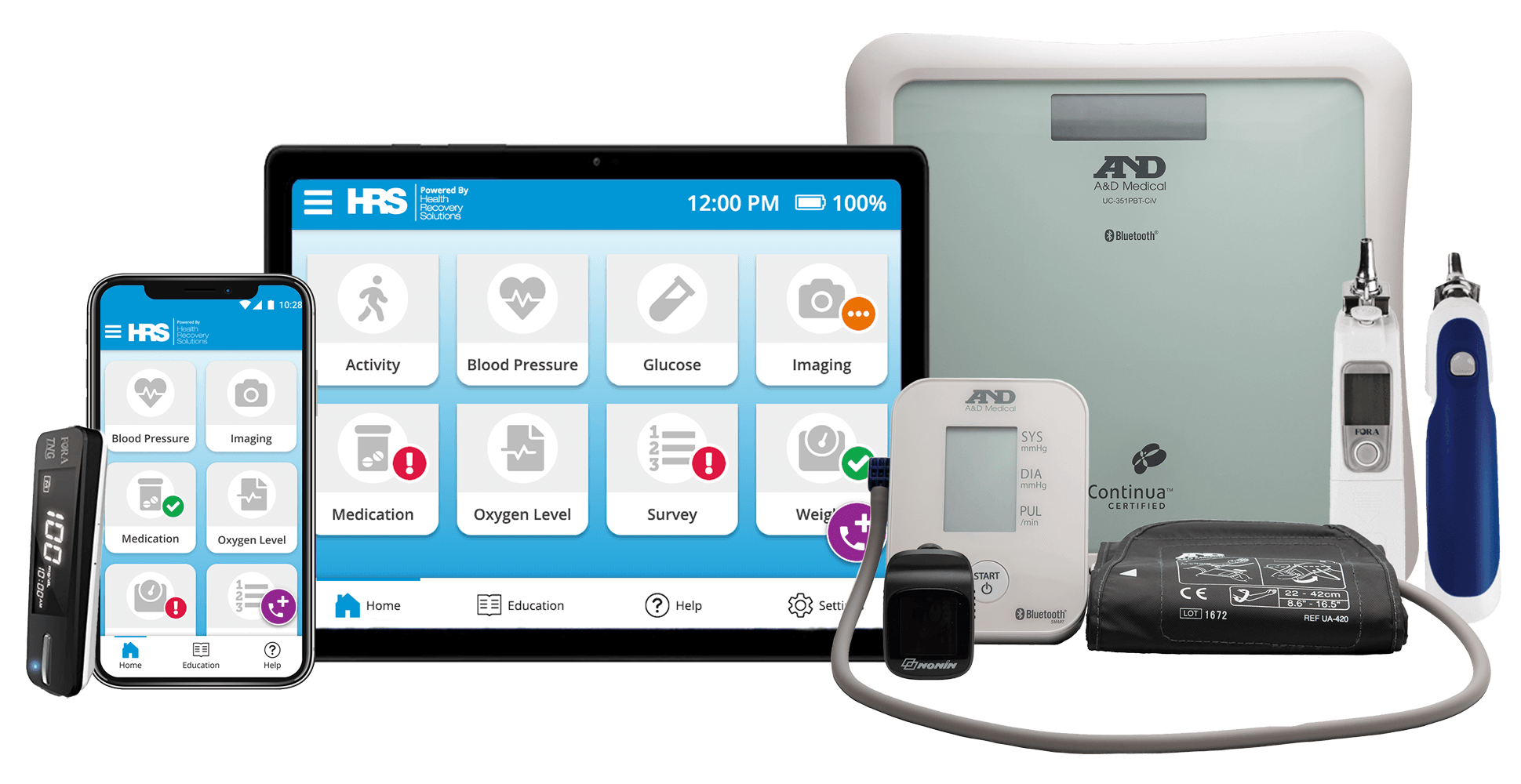
Telehealth and remote patient monitoring (RPM) programs have emerged as powerful tools to address health disparities and promote health equity. By bridging the gap between patients and healthcare providers, these technologies have the potential to improve access to care, enhance clinical outcomes, and empower individuals to take charge of their health.
Telehealth and RPM programs can effectively reduce or eliminate barriers to care, particularly for underserved populations. By providing virtual visit options, these programs alleviate transportation challenges, making healthcare more accessible to individuals in rural areas or those with limited mobility. Additionally, RPM enables the collection of patient data between office visits, allowing for timely interventions and improved clinical outcomes.
These programs advance health equity by:
- Addressing Transportation Barriers - Ability to conduct virtual visits, capture biometrics and transmit patient's clinical data via Bluetooth or Cellular connection creates opportunities to supplement in-person doctor visits and reduce transportation dependencies.
- Improving Clinical-Outcomes - Collection of physiologic and non-physiologic data in between office visits gives visibility and ability to adjust medication or intervene timely to improve clinical outcomes.
- Enabling Health & Digital Literacy - All condition-specific patient educational content within the HRS tablet is created at the 2nd Grade Level with a focus on simplified medical jargon.
- Overcoming Language Barriers - Support for multiple languages on the HRS tablet interface overcomes the language barrier that impacts patients with Limited English Proficiency (LEP) - HRS currently supports 16 languages
- Enabling RPM 'Techquity' - HRS tablets do not depend on patients having their own Wi-Fi networks but rather come readily enabled with cellular Sim Cards used by First Responders in rural settings. This ensures that patients are not marginalized due to lack of connectivity.
- Collecting SDOH Data – Available Pre-Set to help you collect pertinent data
Telehealth and RPM programs have the potential to revolutionize healthcare delivery, promoting health equity and improving access to care for underserved populations. By addressing transportation barriers, enhancing clinical outcomes, enabling health literacy, overcoming language barriers, and ensuring RPM 'Techquity', these technologies can empower individuals to take charge of their health and achieve better health outcomes. As telehealth and RPM continue to evolve, it is crucial to ensure that these programs are designed and implemented in a way that is equitable, accessible, and culturally sensitive.
Innovators in Health Equity
Some healthcare organizations are leading the way with innovative solutions to drive health equity forward. From scholarship programs promoting education to patient-centered programs leveraging telehealth and RPM, organizations are stepping up to advance health equity.
Kaiser Permanente Health Equity Scholars Program
In 2021, Kaiser Permanente, a nonprofit health plan and integrated health care delivery organization and one of America's leading healthcare providers, launched the Kaiser Permanente Health Equity Scholars Program. The program aims to build healthier communities by helping students achieve their dreams of going to college. This scholarship program enables young leaders to pursue a clinical or non-clinical career in the healthcare industry.
Case Study: How Evara Health Uses Telehealth & RPM to Advance Health Equity
Another example of innovative leadership comes from Evara Health, a Federally Qualified Health Center (FQHC) located in Pinellas County, Florida. As an FQHC, Evara handles a slightly different population than your typical healthcare organization.
Their patient census includes:
- 61% racial or ethnic minorities
- 94% patients below 200% the federal poverty line
- 80% patients below 100% the federal poverty line
- 46% Medicaid or CHIP users
- 25% have no insurance at all
Evara never turns anyone away and will provide access to anyone that needs medical care of any kind that they provide.
To better support patients struggling with transportation issues and chronic diseases, Evara sought innovative solutions to improve care delivery. In partnership with HRS, they launched their remote patient monitoring (RPM) program in April 2022.
Today, Evara is expanding their RPM services to cover prenatal (gestational diabetes and hypertension), and postpartum care.
As the only healthcare organization in the state of Florida to receive the HRSA Maternal Health grant, Evara is committed to improving maternal health outcomes by addressing the clinical and health-related social needs of patients at high risk for prenatal and postpartum issues. This includes promoting healthy nutrition, reducing racial and ethnic disparities, and improving maternal health by identifying, monitoring, and measuring prenatal high-risk women.
Pinellas County is home to many special populations that are served by this, including both uninsured and underinsured low-income patients who may be living in poverty, homelessness at-risk, suffering from chronic diseases, or various other areas, like mental health issues.
Learn more about Evara Health’s RPM program in this short video clip or view the full one-hour webinar on "Advancing Health Equity within Hypertensive & Postpartum Patient Populations Using RPM" for a deep-dive into this case study.
For more information on building an RPM program that supports health equity goals for your organization, request your free, personalized demonstration from Health Recovery Solutions today.
The Future of Health Equity
Looking ahead to the future, by understanding health equity, recognizing the current state of health inequity, identifying barriers, and actively engaging the healthcare community, we can work towards closing the gap and ensuring that everyone has the opportunity to achieve optimal health. It is vital to embrace the importance of health equity in the United States and globally, recognizing that CMS health equity and social determinants of health play crucial roles in shaping health outcomes. Through collaborative efforts and a commitment to equity, we can create a more just and healthier society for all.
Ready to deploy telehealth and remote patient monitoring to support your health equity goals? See how our patient-centric solutions can help.
In this white paper, you'll learn about:
- Establishing goals
- Determining your financial plan
- Choosing a technology partner
- Building clinician and patient buy-in
- Other essential factors to consider to ensure your program is successful
