For years, remote patient monitoring (RPM) programs have been proven to deliver multiple benefits, giving clinicians and providers a better picture of their patients’ conditions, helping patients share their vitals from the convenience of their homes, and allowing health care organizations to lower costs while increasing productivity.
When you’re developing your RPM program, it’s important to get a grasp of the key steps involved in the process. It’s also instructive to know which parts of the program an outside vendor like Health Recovery Solutions (HRS) would be responsible for and which components your own organization needs to manage.
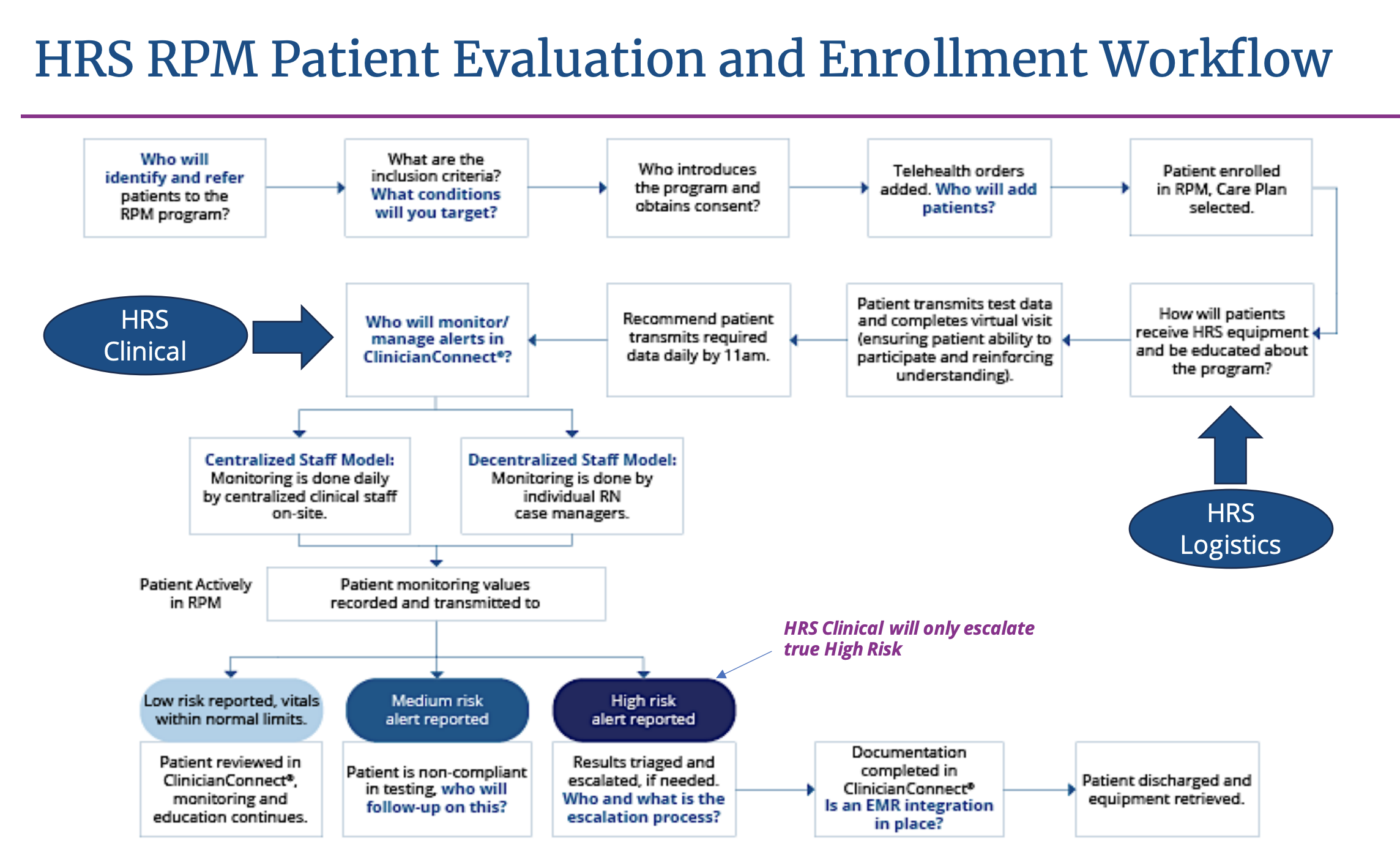
In figure one, we’ve visualized the best practices for RPM enrollment and evaluation. When you break the process down into steps, you can see that it’s not as complicated as you might think.
Watch this 2-minute video clip from a recent webinar to learn more about this workflow or keep scrolling to read about the 5 steps.
Step 1. Patient Identification and Referral
RPM can improve outcomes in a variety of care settings, from cardiology clinics, primary care, Hospital at Home and Home Health to name just a few. The key to identifying the right population or inclusion criteria for an RPM program is to look at your organization’s overall vision and goals. How does RPM help you to meet these goals? Think about the problems you are trying to solve and where RPM can fit in to help address these. Once this is identified the next step is to look at how these patients will receive outreach and get referred into the program. Staff buy-in is the key to success at this stage.
Step 2. Equipment Delivery and Training
The next step to consider as you build this operation, is equipment delivery and retrieval as well as patient training. An organization will need to consider how patients, once identified, will receive, return and get educated on the RPM program. This is a critical step and success here can indicate the level of patient engagement and adherence as they move through the program.
HRS has a great track record of adherence when organizations utilize the HRS Logistics services for their RPM programs. HRS can deliver the equipment anywhere desired via UPS, virtually onboard a patient on how to utilize the equipment, educate on the program and get consent. We can then retrieve the equipment as directed, once the patient is discharged. We can own this process from end-to-end, if needed.
Step 3. Patient Results
Once patients are enrolled and onboarded to the RPM program, they will begin to test their vital signs, answer survey questions and engage in educational video and pdf content throughout the program. The data obtained from these daily interactions will be delivered to the HRS clinical platform called ClinicianConnect. The information received from the patients daily will need to be reviewed timely to ensure timely patient intervention and escalation to providers. It is important to understand your staffing pre-RPM to know who and how this process will be achieved.
There are many ways to accomplish this and we describe two common operations below:
- Centralized model. In this model, all RPM data (from all programs within your organization) flows to a specific individual or an RPM department within your organization. This person/team will have clear roles and responsibilities and understand the process of communication to providers for timely escalation. The staff working in the RPM central department will not have additional duties outside of this program.
- Decentralized model. Here, all RPM data is distributed to each clinician or department responsible for their assigned group of patients. This model has staff members performing their current duties and adding this task to those roles and responsibilities already in motion. While not as common, this model can be successful.
If your organization is dealing with staff shortages, HRS can help. HRS has a program called CareConnect that provides clinical monitoring services up to 24/7 to assist your team in the tasks of an RPM operation. Our team will be responsible for receiving, interpreting and intervening for all high-risk results from vital sign readings to survey question answers. CareConnect acts as the initial clinical triage and patient outreach.
Boost Your Staff: How Telehealth Can Help Mitigate Healthcare Staffing Shortages
This 45-minute webinar explores the impact of staffing shortages on the healthcare industry and how Lee Health is using a centralized model for telehealth & RPM to address challenges.
Step 4. Response to Patient Results
High risk patients are engaged and readings are being received by your clinicians, they will need to be addressed timely. The key to great results is timely intervention, escalation and treatment. This timely care will get the patient treated at the right level of care at the right time, keeping them home and their disease under control. Plan to create a protocol/process that defines timely intervention, escalation process (who to contact and how) and treatment (are there any standard protocols you can create that will allow nurses to instruct patient on the physicians orders in the standard protocol-ie: patient gained 5lbs in 7 days-double your diuretic for 2 days).
As patients transmit their daily results, the RPM team will see the readings categorized as below in HRS. These categories are selected based on the parameters the RPM program decided upon before the program went live.
- Low risk. Patient vitals are within normal ranges.
- Medium risk. In most cases this is selected by the program team to indicate a patient’s nonadherence >2 days. It is recommended the RPM team member reach out to the patient to investigate the reason for the nonadherence.
- High risk. Results are reported that require clinical intervention. Highest Priority.
Step 5. Discharge from the Program
A key to decreasing 30- and 60-day readmissions is knowing and documenting when a patient should be discharged from the program. Discharging a patient too early can increase the incident of readmission and discharging a stable patient too late can prevent another higher risk patient from receiving a referral into the program.
Once a patient is identified and meets the criteria for discharge, a plan for retrieving the equipment is needed. HRS can help with retrieval through our logistics program.
Some suggestions to know when to discharge/criteria for discharge would be the following:
- Patient stable on medications without adjustments in the last 14 days
- No readmission in the last 30 days
- Patient has a plan after discharge to continue to monitor their disease process
Throughout this process, Health Recovery Solutions can keep your RPM program operating smoothly, efficiently and accurately.

End-to-End RPM Program
From referral to discharge, the team of experts at Health Recovery Solutions is here to help you and your patients succeed. Contact us today for a personalized demonstration.