A recent study conducted by BJC HealthCare and the Washington University School of Medicine delved into the realm of remote patient monitoring (RPM), exploring its potential benefits for individuals with congestive heart failure (CHF) and chronic obstructive pulmonary disease (COPD) within an Accountable Care Organization (ACO).
Let's review the key findings and implications of this study.
The Study Setup
The study, conducted between February 2021 and December 2021, focused on the integration of RPM for patients discharged from the hospital with CHF or COPD. The RPM intervention included vital sign monitoring equipment, a tablet with symptom tracking software, educational material, and nurse oversight. Health Recovery Solutions (HRS), provided RPM equipment distribution and between-patient cleaning of devices and materials but played no role in the design, oversight, or analysis of this study. 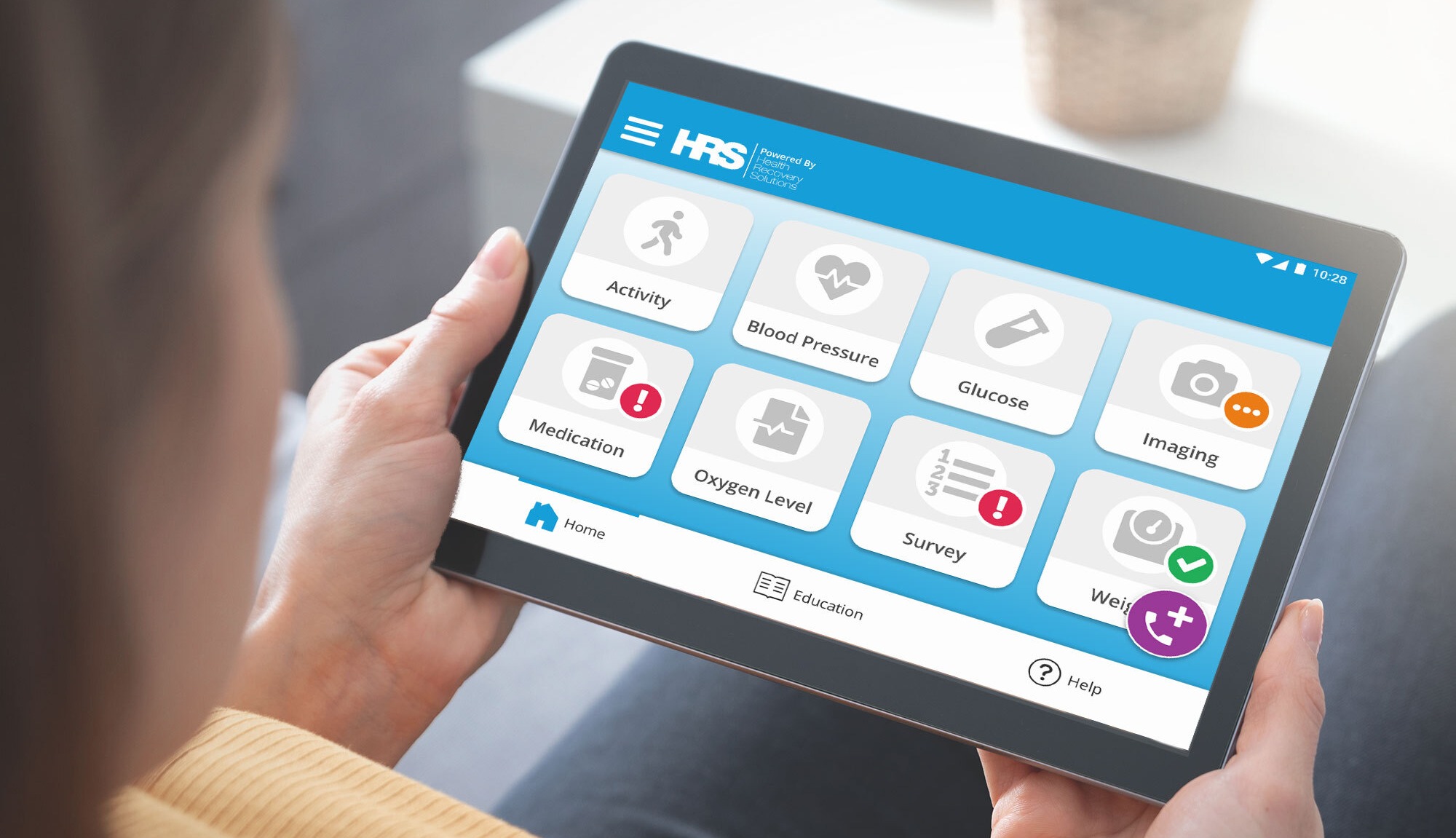
Key Findings
Out of 361 patients offered RPM, 140 opted to enroll, with a median RPM enrollment duration of 54 days. The study's primary outcomes were centered around a composite of death, hospital admission, or emergency care visits within 180 days of eligibility. While there was no significant difference in the frequency of the primary composite outcome between the RPM and control groups, the study revealed a notable reduction in 6-month mortality among RPM-enrolled patients (6.4% vs. 17%).
Adjusted analyses, which accounted for potential confounding factors, suggested a nonsignificant decrease in the odds of the primary composite outcome and lower 6-month mortality with RPM enrollment. Subgroup analysis focusing on patients with CHF showed a significant decrease in 180-day mortality in the RPM group, indicating that the benefits might vary among different patient populations.
Sensitivity analyses supported the robustness of the findings, and an exploration into RPM engagement hinted at a potential dose-dependent relationship with improved outcomes. Despite the non-randomized nature of the study and the likelihood of confounding by indication, the use of modern statistical methods provided confidence in the results.
Implications for Patient Care
The study's findings suggest that RPM enrollment may be associated with decreased odds of 6-month mortality, particularly for patients with CHF. This opens up new possibilities for leveraging technology to enhance patient outcomes, especially for those with chronic conditions requiring post-hospitalization care.
Improving Patient Outcomes with RPM
The study provides valuable insights into the potential benefits of remote patient monitoring, shedding light on improved health outcomes for the selected patient populations. With the continued advancement of technology and the integration of these solutions into healthcare practices, we are witnessing a transformative shift in how we manage chronic conditions and deliver personalized care to those who need it most.

About this study
Post-hospitalization remote patient monitoring (RPM) has potential to improve health outcomes for high-risk patients with chronic medical conditions. The purpose of this study is to determine the extent to which RPM for patients with congestive heart failure (CHF) and chronic obstructive pulmonary disease (COPD) is associated with reductions in post-hospitalization mortality, hospital readmission, and ED visits within an Accountable Care Organization (ACO).