Medication non-adherence can have a more direct impact on patient outcomes than specific treatments themselves, playing a key role in patients’ quality and length of life and in the overall costs seen by patient and industry alike.
As discussed in our previous blog on medication adherence, it is estimated that half of those taking medications in the US aren’t following doctors’ orders, driving the nation’s healthcare bill upwards by about $310 billion in avoidable costs and $100 billion in avoidable hospitalizations.
The issue is especially common among those taking multiple medications with complex regimens and schedules. In fact, the top 1 percent of high-acuity chronic disease patients accounts for 23 percent of that healthcare bill, or about $107,000 per year per patient.
But where does the responsibility fall? The patient? The provider?
The answer: both.
Patients often fail to understand the consequences of medication non-adherence, both for themselves and for the healthcare system at large. They may feel unmotivated to follow their prescription regimen or the complexity and cost of such a regimen may intimidate and dissuade them from taking medication altogether.
Providers may fail to acknowledge the reasons for patient non compliance, such as the patients’ lack of understanding to follow-up on medication plans, or even the fact that change for patients can be hard. In any case, hospitalizations and emergency department visits that result from poorly optimized care may result in no reimbursement for medical treatment.
How do we change medication non-adherence?
By providing patients with a remote patient monitoring (RPM) and telehealth platform to help.
Medication non-adherence is less of a concern in hospital and healthcare facilities as access to and distribution of medications are more strictly controlled than in a patient’s home environment.
Medication non-compliance occurs most often when a patient returns home from the hospital or clinic. This transition of care period is where education on the importance of medication adherence becomes integral to the patient's success. Trust between patient and provider and a blame-free environment that provides encouragement to patients must be established.
RPM platforms provide patients with the tools they need—medication reminders, regular virtual visits, and custom medication-specific education—to reduce medication non-adherence and positive behavior change.
Medication Therapy Management (MTM)
A core area of focus for chronic disease management has been medication therapy management (MTM), with telehealth and remote patient monitoring at the forefront. Access to digital information and communication technologies to remotely access healthcare services can successfully address continued issues with medication non-adherence.
Digital pillboxes, easy access to reconciled medication lists, and personal reminder platforms can each reduce patient non compliance and thereby improve patient outcomes. Even the simplest form of telemedicine, the telephone, has the power to deliver essential support to patients who are at high risk of medication non-adherence.
As it is estimated that 77% of Americans own a smartphone of some kind, text messaging is a key virtual strategy worth exploring.
In a meta-analysis that analyzed different text-messaging designs that were studied in 16 random controlled trials, researchers found that text messaging doubled the odds of medication adherence and improved overall adherence rates by 17.8%. Half of the trials incorporated daily text messages and 31% were personalized for patients, indicating that text messaging can serve as a powerful tool for combating medication non-adherence.
How HRS Can Help with Medication Non-Adherence
HRS' solution suite—PatientConnect Complete, Core, Mobile, and Voice, all help patients adhere to their medication regimen.
Let's consider a patient example.
Stacy is a 77 year-old patient who was recently discharged from the hospital after an exacerbation in heart failure symptoms. Stacy also has diabetes which requires multiple medications daily, in addition to her CHF medications prescribed by her physician.
While in the controlled environment of the hospital, Stacy was compliant to her medications, but now she is returning home where she lives alone. Stacy will be receiving home health visits, but her nurses are concerned about whether she'll adhere to her medications as prescribed. If Stacy doesn't adhere to her medication, she runs the risk of returning to the hospital.
The home health agency serving Stacy enrolls her in their agency's telehealth program. Immediately upon discharge, Stacy is sent home with PatientConnect Complete, HRS' comprehensive telehealth kit that includes a tablet and Bluetooth biometric peripherals. The tablet is pre-downloaded with a care plan specific to Stacy's condition that includes medication reminders, symptom surveys, and communication tools for Stacy to actively communicate with her clinician through video, phone, and chat.
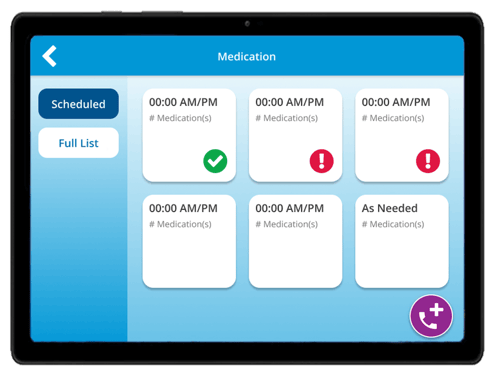 An example of a medication reminder on the HRS tablet.
An example of a medication reminder on the HRS tablet.
Through the tablet, Stacy receives medication reminders for all medications prescribed. When she takes the medication, she records the action on the tablet. Daily, Stacy's nurse can see whether Stacy is taking her medications as prescribed and contact her if concerned about her compliance or simply to check in.
Overtime, both Stacy and her nurse can track trends in behavior change. When Stacy has a question about one of her medications, her nurse is available at a click of a button through the tablet. Telehealth helps Stacy avoid medication non-compliance resulting in controlled symptoms, improved outcomes, and a reduced risk of readmission.
Want to learn more about how the HRS solution can help patients improve medication adherence? Visit our solutions page.
Ready to get started with telehealth and RPM?
