Incorporating telehealth and telerehabilitation into the care continuum poses a large opportunity for Total Knee Arthroplasty (TKA) recovery. A recent study out of Duke found that a virtual PT platform, called VERA, resulted in significantly lower 12-week postoperative costs and was effective and safe for treating pain and reducing rehospitalization among TKA patients.
Reducing Costs and Improving Access with Telerehabilitation
There is an urgent need within US healthcare to address the increasing rates of Total Knee Arthroplasty (TKA). The United States has the highest incidence of TKA in the world, with the orthopedic procedure performed on over 700,000 patients annually – a figure that is projected to increase 143% by 2050 (this is the highest incidence of TKA in the world).
Physical therapy for rehabilitation has proven to be an effective post-operative recovery method for TKA. Therapists assign and monitor patient exercises to help ease joint pain and restore physical functionality, ultimately improving the patients’ quality of life and accelerating recovery time. The current nationwide shortage of therapists combined with expensive out-of-pocket costs for patients will make it difficult to continue meeting the needs of this growing patient population via traditional physical therapy.
By utilizing telehealth, therapists can host virtual visits and remotely monitor their patients’ rehabilitation, providing a low-cost and clinically effective option that increases access to care. Virtual Exercise Rehabilitation In-home Therapy: A Randomized Study (VERITAS), released in November 2019 by Duke University, was designed to examine the cost and clinical noninferiority of a virtual PT program when compared to traditional care after TKA. The virtual PT platform, called VERA, resulted in significantly lower 12-week postoperative costs and was effective and safe for treating pain and rehospitalizations. These findings have important implications for patients, health systems, and payers as they continue to seek innovative ways to make physical therapy more accessible.
Managing Patients with TKA
TKA is often assigned to patients suffering from joint pain due to osteoarthritis, which is the most common type of arthritis found among elderly patients. The degenerative joint disease impairs physical functionality and restricts mobility, making casual daily activities an uncomfortable challenge. TKA is reserved for more severe cases of osteoarthritis, and usually comes into play once the patient has already tried more conservative treatment plans – ie. medication, physical therapy and/or cortisone injections. Musculoskeletal (MSK) conditions such as osteoarthritis are the leading cause of disability in the US, affecting more than half of the population. Although the postoperative recovery process can be difficult and costly, TKA is a popular procedure for relieving pain and improving the quality of life for patients suffering from arthritis or other joint pain.
For total joint replacement (TJR) surgeries, telehealth has the ability to be a safe, low-cost tool for treating patients during recovery. Aging populations are staying active later in life, requiring solutions that will reduce the expensive cost burden on patients and providers without negatively impacting patient outcomes. Here are some other key figures to keep in mind as we explore the future impact of rising TKA rates on:
- 700,000+ knee replacements performed annually since 2010
- The US has the highest IR of knee arthroplasty in the world: 235 procedures/100,000 people
- Among older patients, the volume of TKAs has already doubled from 1991 to 2010
- Research predicts 3.5 million TKAs / year predicted by 2030
- Volume of TKAs in the US expected to increase 143% by 2050
Physical therapy is an important and effective treatment program for postoperative patients recovering from TKA. Overcoming the financial and clinical barriers that restrict patients from receiving traditional physical therapy is at the center of unlocking this critical access to care.
VERITAS: Comparing Virtual PT with Traditional PT
The VERITAS project from Duke University found positive results supporting the advancement of virtual PT technology, citing significantly lower costs after TKA while providing similar effectiveness. In the study, tele-rehabilitation using virtual PT was found to make healthcare more convenient, effective, and affordable than traditional care, enabling improved access through reduced costs. The VERITAS study was the first randomized controlled trial to examine costs and clinical outcomes for this type of telehealth physical therapy program. Their results demonstrate that virtual PT with tele-rehabilitation for skilled clinical oversight significantly lowers healthcare costs after TKA without affecting the safety or quality of patient care. By taking a closer look at VERITAS and other virtual PT studies, we can better understand the various benefits of introducing telehealth to help manage patients recovering from total joint replacement surgery.
Implementing Virtual Physical Therapy
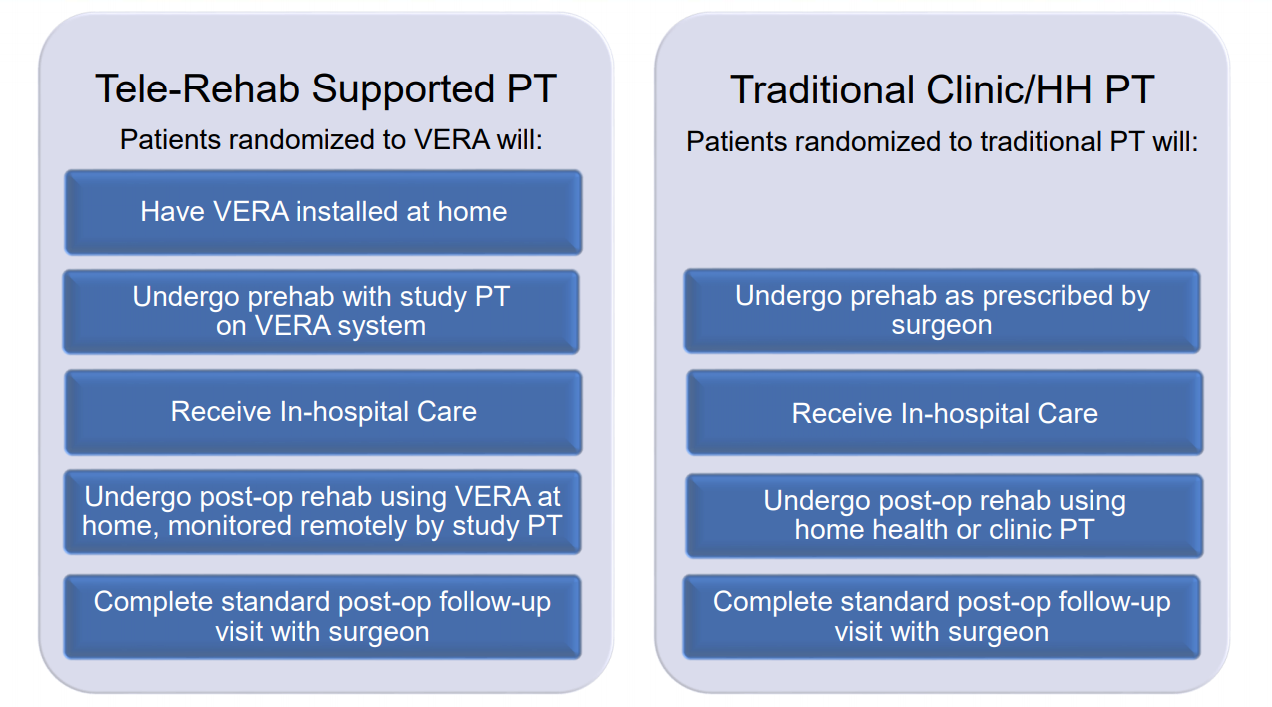
VERITAS, which ran from November 2016 through November 2017, primarily aimed to evaluate total costs 12 weeks after discharge for TKA. Other patient-centered outcomes included clinical effectiveness and safety of virtual PT compared to traditional physical therapy care. Almost 300 patients completed the study, and baseline information was obtained through physical function performance tests (assessed via KOOS – knee injury and osteoarthritis outcome score). Patients also set personal recovery goals and recorded their progress in a diary, improving engagement with disease self-management. Traditional physical therapy was either conducted at a clinic or in the patient’s home, while the virtual physical therapy group had a system called VERA installed in their homes.
VERA is a tele-rehabilitation platform that uses 3-D motion-capture technology to measure patient mobility and provide feedback on exercise performance. Patients had the virtual system installed in their home prior to surgery after demonstrating the ability to use VERA to receive exercises at home, enabling patients to begin the program immediately after discharge from the hospital. Featuring a virtual avatar guide, patients had assistance working through exercises with the aid of visual and audible instructions. Cameras were used to track patient exercises live, and the recorded videos could be viewed later by physical therapists in order to review progress and adjust treatment plans. Patients can view their own progress, while PTs can adopt a centralized care model to remotely monitor the data asynchronously. With virtual PT, patients have the ability to schedule a virtual visit with their provider to communicate in real time and receive recommendations regardless of provider location. These factors contribute to overall improved access and support for a larger number of patients, while also reducing total cost for providers.
Benefits of Virtual PT for Telerehabilitation
VERA remotely monitored patients to measure activity, performance, exercise quality, and adherence. The baseline results for 306 randomized patients were not significantly different between the two groups, but the key findings related to cost savings present a massive growth opportunity for providers via telerehabilitation. By augmenting traditional PT with telerehabilitation, providers are able to support greater access to care for patients recovering from TKA.
VERITAS Results:
- Total cost savings of $2,745 per patient in a bundle
- Total readmissions reduced by 60%
- Increases adherence to home exercise programs from 3.3 days/week to 5.9
- As safe and effective as traditional PT
- Virtual PT more beneficial for knee function during sports and recreation
From this data, researchers concluded that “these findings have important implications for patients, health systems, and payers. Virtual PT with clinical oversight should be considered for patients managed with TKA.”
The Future of Recovery with Tele-rehabilitation
How do we scale this? Telehealth policy makes a huge impact on cost savings; bundled payments reduce cost without affecting the quality of care. Cost, convenience, and access to physical therapists rely on using technology to overcome geographic barriers.
Other studies using tele-rehabilitation have also demonstrated similar patterns of non-inferiority between traditional and virtual physical therapy. Earlier in 2019, researchers from Yale University implemented virtual PT for patients recovering from total joint surgery (for knee and hip replacements). The study, which also acknowledges the increasing demand for TKA in the US, successfully demonstrates the feasibility of utilizing a tele-rehabilitation program without compromising clinical quality and patient satisfaction.
There's an incredible opportunity for incorporating telehealth into physical therapy. Telehealth enables PTs to delivery high quality, convenient care, while also improving clinical workflow and reducing costs. As the incidence of TKA increases and consequentially the need for PT, organizations will be required to innovate on how they deliver care to their patients.
References:
Inacio MCS, Paxton EW, Graves SE, Namba RS, Nemes S. “Projected Increase in Total Knee Arthroplasty in the United States – an Alternative Projection Model.” Osteoarthritis and Cartilage, vol. 25, no. 11, 2017., doi:10.1016/j.joca.2017.07.022.
Bettger, Janet Prvu, et al. “Effects of Virtual Exercise Rehabilitation In-Home Therapy Compared with Traditional Care After Total Knee Arthroplasty.” The Journal of Bone and Joint Surgery, vol. 102, no. 2, 2019., doi:10.2106/jbjs.19.00695.
Kuether J, Moore A, Kahan J, Martucci J, Messina T, Perreault R, Sembler R, Tarutis J, Zazulak B, Rubin LE, O'Connor MI. “Telerehabilitation for Total Hip and Knee Arthroplasty Patients: A Pilot Series with High Patient Satisfaction”. HSS J. 2019 Oct;15(3):221-225. doi: 10.1007/s11420-019-09715-w. Epub 2019 Aug 21
Moffet, Hélène, et al. “Telerehabilitation After Total Knee Arthroplasty: Results from a Randomized Controlled Trial”. Telemedicine and e-Health. 2017., doi:10.1089/tmj.2016.0060
Carvalho E, Bettger JP, Goode AP. “Insurance Coverage, Costs, and Barriers to Care for Outpatient Musculoskeletal Therapy and Rehabilitation Services”. N C Med J. 2017 Sep-Oct;78(5):312-314. doi: 10.18043/ncm.78.5.312.
Duke University. “Virtual vs. Traditional Physical Therapy Following Total Knee Replacement” ClinicalTrials.gov, 2019, clinicaltrials.gov/ct2/show/NCT02914210.
Fingar KR, Stocks C, Weiss AJ, Steiner CA. “Most Frequent Operating Room Procedures Performed in U.S. Hospitals, 2003–2012.” HCUP Statistical Brief #186. 2014. https://www.hcup-us.ahrq.gov/reports/statbriefs/sb186-Operating-Room-Procedures-United-States2012.pdf.