Welcome to part 2 of our blog series on telehealth reimbursement. In part 1, we discussed the different reimbursement models for telehealth services and addressed some of your burning reimbursement questions. Now, in part 2, we will take a closer look at the Centers for Medicare & Medicaid Services (CMS) reimbursement codes for chronic care management (CCM), remote patient monitoring (RPM), and remote therapeutic monitoring (RTM) services.
We will also explore the new home health agency G-codes and examine Health Recovery Solutions' automated reimbursement report.
With the unprecedented acceleration of telehealth services due to the COVID-19 pandemic, it's more important than ever for healthcare providers to have a solid understanding of telehealth reimbursement codes and regulations to ensure they can continue to provide high-quality care to their patients remotely while generating new revenue.
In this post, we’ll cover:
- Chronic Care Management (CCM) CPT Codes
- Remote Patient Monitoring (RPM) CPT Codes
- New Home Health Agency G-Codes for RPM
- Remote Therapeutic Monitoring (RTM) CPT Codes
- HRS’ Automated Reimbursement Report

2023 Telehealth Reimbursement Advancements
In this 30-minute session, HRS' Vice President of Revenue Cycle Management presented on the 2023 updates to telehealth reimbursement rates and reviewed how HRS can support your reimbursement efforts.
Chronic Care Management (CCM) CPT Codes
Chronic care management (CCM) helps patients with chronic conditions manage their health and prevent complications. There are a number of different CCM CPT codes that can be used to bill for these services.
The most common codes are:
- 99487: This code is used to bill for complex CCM services that are provided by clinical staff Complex CCM services are those that require moderate to high complexity medical decision-making
- 99489: This code is used to bill for additional 30 minutes of complex CCM services
- 99490: This code is used to bill for non-complex CCM services that are provided by clinical staff Non-complex CCM services are those that do not require moderate to high complexity medical decision-making
- 99439: This code is used to bill for additional 20 minutes of non-complex CCM services.
- 99491: This code is used to bill for CCM services that are provided personally by a physician or other qualified health care professional
The reimbursement rate for CCM services varies depending on the code that is used. The CMS national average reimbursement rate for CPT code 99487 is $133.18. The average reimbursement rate for the subsequent codes varies from around $47 to $85.
It is important to note that these are just national average reimbursement rates. The actual reimbursement rate that you receive may be higher or lower, depending on your specific contract with the payor.
Billing for CCM and RPM Together
CCM can be billed in conjunction with remote patient monitoring (RPM). Since RPM services can help to identify and prevent complications in patients with chronic conditions, billing for CCM and RPM together can create value for both patients and providers. For patients, it can mean that they receive more comprehensive care that is better coordinated across different providers. For providers, it can mean that they bill for both CCM and RPM in the same month to get the most ROI for their services.
Remote Patient Monitoring (RPM) CPT Codes
Let’s get into the remote patient monitoring (RPM), or remote physiological monitoring, codes. Watch this 6-minute clip from the 2023 Telehealth Reimbursement Advancements Webinar or keep scrolling for a quick overview. In the video clip, Charika Wilcox-Lee, Vice President of Revenue Cycle Management at HRS, discusses the RPM CPT Codes and RPM Billing Guidelines.
There are a number of different RPM CPT codes that can be used to bill for these services.
The most common codes are:
- 99453: This code is used to bill for the initial setup and patient education of RPM equipment. It is a one-time billable fee
- 99454: This code is used to bill for the supply of the RPM device, the collection, transmission, and reporting of data. This code can be billed every 30 days
- 99457: This code is used to bill for the first 20 cumulative minutes of RPM services. This code can be billed by clinical staff, a physician, or other qualified healthcare professional (QHCP)
- 99458: This code is an add-on code that can be used to bill for additional 20-minute increments of RPM services. This code can only be billed by a physician or QHCP
- 99091: This code is used to bill for the collection and interpretation of data by a physician or QHCP for 30 minutes. This code can only be used by physicians or QHCPs
It is important to note that these are just the most common CPT codes for RPM services. There are other codes that may be appropriate depending on the specific services that are provided.
RPM Billing Guidelines
There are a number of billing guidelines that must be followed when billing for RPM services. Some of the most important guidelines include:
- 99453 can only be billed once per patient per episode of care
- 99454 can only be billed once per patient per month
- 99457 and 99458 can only be billed by a physician or QHCP
- 99091 can only be billed by a physician or QHCP
- 99453, 99454, 99457, and 99458 cannot be billed for the same patient on the same day
Billing for RPM Devices
Billing codes 99453 and 99454 are both device-based codes that are used to bill for RPM services. Bluetooth-enabled RPM devices connect directly with the RPM application, enabling patients to monitor their vitals and biometrics in real-time, and communicate with their providers via virtual visits and secure messaging, all from the convenience of their personal device or pre-configured tablet.
The billing guidelines for code 99453 require 16 days of reported Bluetooth metrics from these devices. That means we’re getting those readings in from the RPM devices for blood pressure or weight or glucose and we're recording at least 16 readings within a 30-day period. If the patient has COVID-19, the criteria is a little different. It’s only two Bluetooth active days during the Public Health Emergency. Even though the PHE is ending on May 11th, this rule will continue until the end of the year.
CPT code 99454 follows the same guidelines and is billable every 30 days.
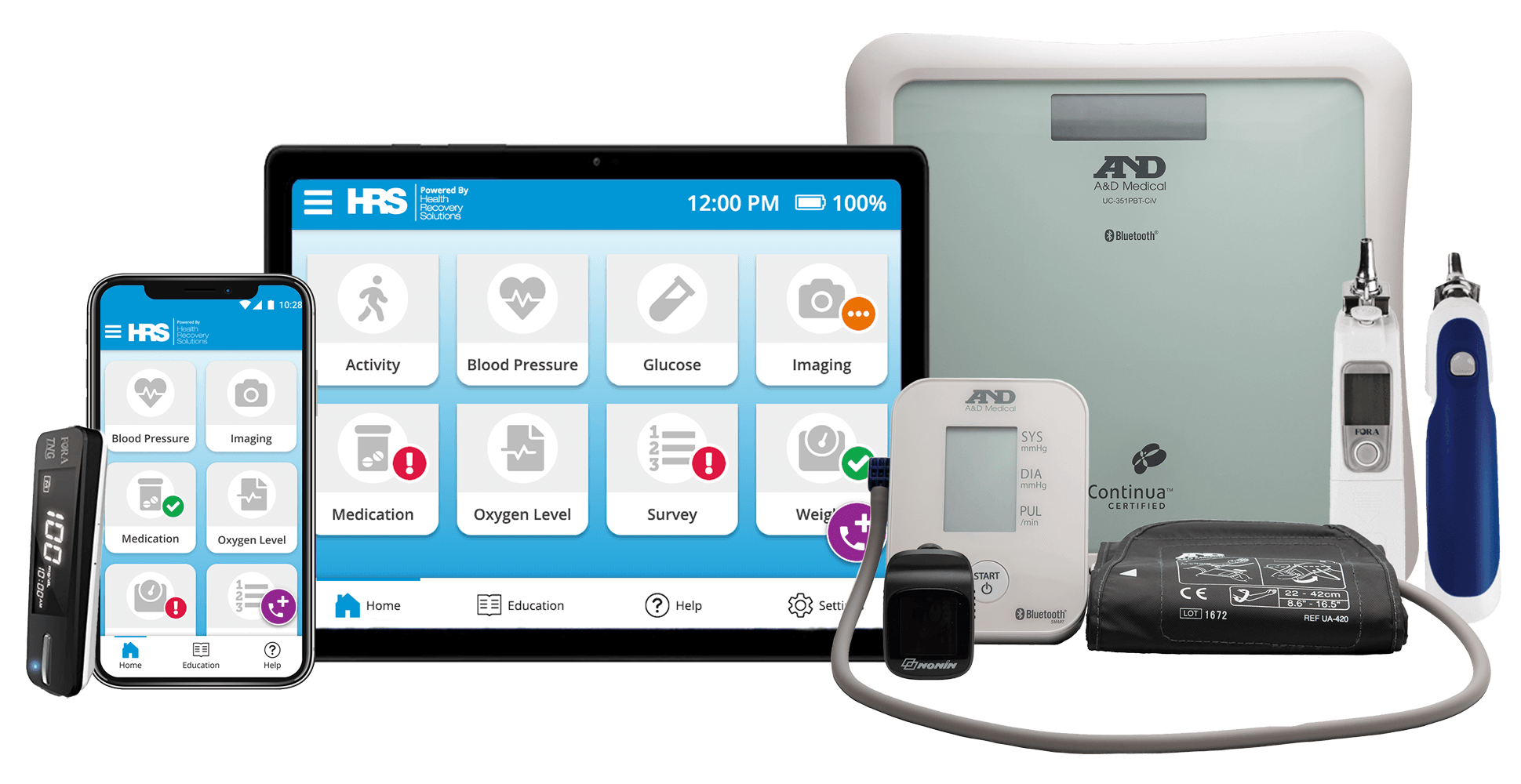
7 Common Remote Patient Monitoring Devices
There are many remote patient monitoring devices available on today’s market. Learn more about 7 devices that we commonly see used in remote patient monitoring programs.
Billing for RPM Care Management
Codes 99457 and 99458 are both time-based codes that are used to bill for the time a healthcare provider spends on care management and interactive communication with a patient.
CPT code 99457 is your primary time spent code. This code requires 20 minutes of care management and interactive communication.
CMS defines care management as reviewing the dashboard, looking at those metrics that are coming in on a consistent basis, reviewing the patient's chart along with that interactive communication piece. Interactive communication can be video visits or audio visits with the patient talking about their care plan. All of that is incorporated into code 99457 and is billable every 30 days.
CPT code 99458 is an add-on code. This code covers any additional 20 minute-increments of care management and interactive communication. This cannot be billed as a standalone code. It must be billed in conjunction with 99457.
Let's say you spent 60 minutes with the patient, you would bill one unit of 99457 plus two units of the 99458 to cover that 60-minute timeframe. Note that incident-to rules apply to general supervision. Your clinical staff can engage with the patient but the supervising physician listed on the reimbursement claim is responsible for the services.
It is important to review the billing guidelines carefully before billing for RPM services or work with a trusted RPM vendor that provides reimbursement support. Failure to follow the guidelines could result in denial of payment.
New Home Health Agency G-Codes for RPM
CMS has implemented new G-codes that will be used for home health agencies to report RPM services. These codes are informational only and will not be reimbursed by CMS. However, they are required for all HHA RPM programs starting on July 1, 2023.
The three new G-codes for home health agencies are:
- G0320: Video visits with patients to discuss their care plan
- G0321: Audio communications with patients to discuss their care plan
- G0322: Collection of physiological data that is stored and transmitted
These codes will be reported on a monthly basis. To make it easier for providers to comply with this new requirement, we will be populating these codes on our reimbursement report starting in May. This will give you the information you need to submit these claims to CMS.
We recommend that you start submitting test claims prior to the July 1st deadline to ensure that you are using the correct codes and that your claims are being processed correctly.
Remote Therapeutic Monitoring (RTM) CPT Codes
Remote therapeutic monitoring (RTM) is similar to RPM, but it covers two systems: respiratory and muscular skeletal.
The CPT codes for RTM are:
- 98975: Initial setup and patient education on equipment
- 98976: Supply of the RTM device, collection, and reporting for respiratory
- 98977: Supply of the RTM device, collection, and reporting for muscular skeletal
- 98980: First 20 minutes of RTM time spent. This code is similar to RPM, with the 98981 being an add-on code for every additional 20-minute increment
What makes RTM different from RPM is that patients are able to self-report in an RTM program. Bluetooth active days are not required, but 16 days of collected data and measures are required.
It is important to note that RTM and RPM cannot be billed together at this time. CMS has received comments advising that these two services are different and should be able to be billed together, but this is not the case at the current time. Hopefully, this will change in the future.
CMS has also made some changes to the RTM codes, adding some H pick codes. However, these codes are not mandatory at this time. CMS has given providers until January 1, 2024 to implement these new codes.
We will provide more information about these changes and the benefits of billing RPM and RTM together in the future.
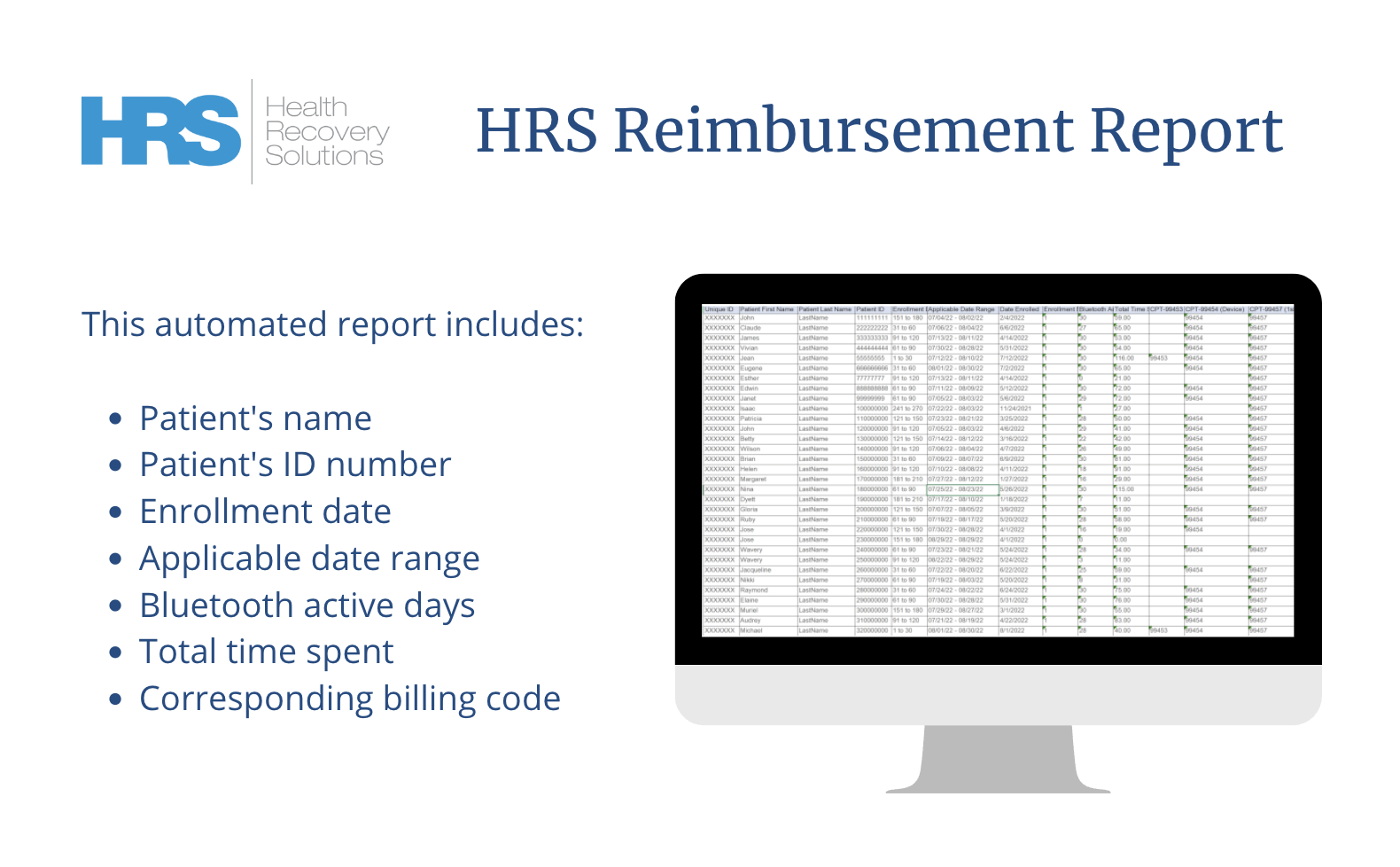
HRS’ Automated Reimbursement Report
Our automated reimbursement report provides you with the information you need to submit claims for remote patient monitoring (RPM) services. Watch this 2-minute clip from the 2023 Telehealth Reimbursement Advancements Webinar for a quick overview. In the video, Charika Wilcox-Lee, Vice President of Revenue Cycle Management, explores a sample Reimbursement Report from HRS.
The report includes the following information for each patient:
- Patient's first name, last name, and patient ID number
- Enrollment date
- Applicable date range
- Bluetooth active days
- Total time spent
If total time spent is being captured within our system, ClinicianConnect®, we are able to report on this information for you. If total time spent is only being captured in your EMR, we cannot capture it on this report. We recommend that you capture total time spent in ClinicianConnect® and integrate it with your EMR for a smoother process.
The report also includes the following information:
- CPT device codes
- Number of units billed for each CPT code
Based on this information, you can determine what codes can be billed for each patient. We send this report to our clients by the fifth business day of the following month to help you get your claims out the door. The report also helps you to identify proper usage of codes based on the billing guidelines.
How HRS Helps with Telehealth Reimbursement
In conclusion, CCM, RPM, and RTM are valuable tools that can help providers to manage their patients' chronic conditions and improve their health outcomes using the latest telehealth technology. The billing guidelines for these services can be complex, but by following the guidelines in this post, providers can ensure that they are correctly reimbursed for the services that they provide.
HRS help providers navigate the reimbursement process with our in-house team of reimbursement specialists and automated reimbursement report. The HRS Reimbursement Report can help healthcare providers to streamline the billing process for RPM services. The report provides providers with the information necessary to submit reimbursement claims for RPM services, and it also helps providers to identify proper usage of CPT codes based on the billing guidelines.
Calculate Your Potential Reimbursement
Our team of reimbursement specialists is dedicated to helping our partners receive reimbursement for RPM services. We invite you to use our interactive calculator to see how RPM can be a new revenue stream for your organization.