Overview
CommonSpirit Health at Home Rapidly Expands Remote Patient Monitoring
CommonSpirit Health at Home is a full service healthcare organization that believes the best place for someone to get better, and faster, is in their own home.
In 2018, CommonSpirit Health at Home first piloted a remote patient monitoring (RPM) program with the primary goal of changing patient behavior to reduce rehospitalizations and emergency department (ED) visits.
In 2020, in response to the pandemic, CommonSpirit Health at Home expanded their pilot program, offering RPM services to home health patients in 12 states across 40 locations and expanded enrollment to numerous conditions including CHF, COPD, hypertension, diabetes, post-surgical, pneumonia, oncology, and COVID-19, among others.
Challenge
To engage patients and prevent hospital readmissions, CommonSpirit Health at Home aimed to enroll the highest-risk patients with multiple comorbidities, a history of medication and symptom mismanagement, and elevated risk for hospital readmission.
Since expanding the initial pilot program, CommonSpirit Health at Home has outlined additional goals for the Health at Home program:
- Reduce hospital readmissions and ED visits
- Increase clinical touch points through the use of virtual visits
- Increase in patient satisfaction
- Enhance pain and medication management for chronic care patients
Get Started with Remote Patient Monitoring
Connect with an HRS Digital Health Advocate to learn more about the industry-leading remote patient monitoring and logistics options available to your organization.
Solution
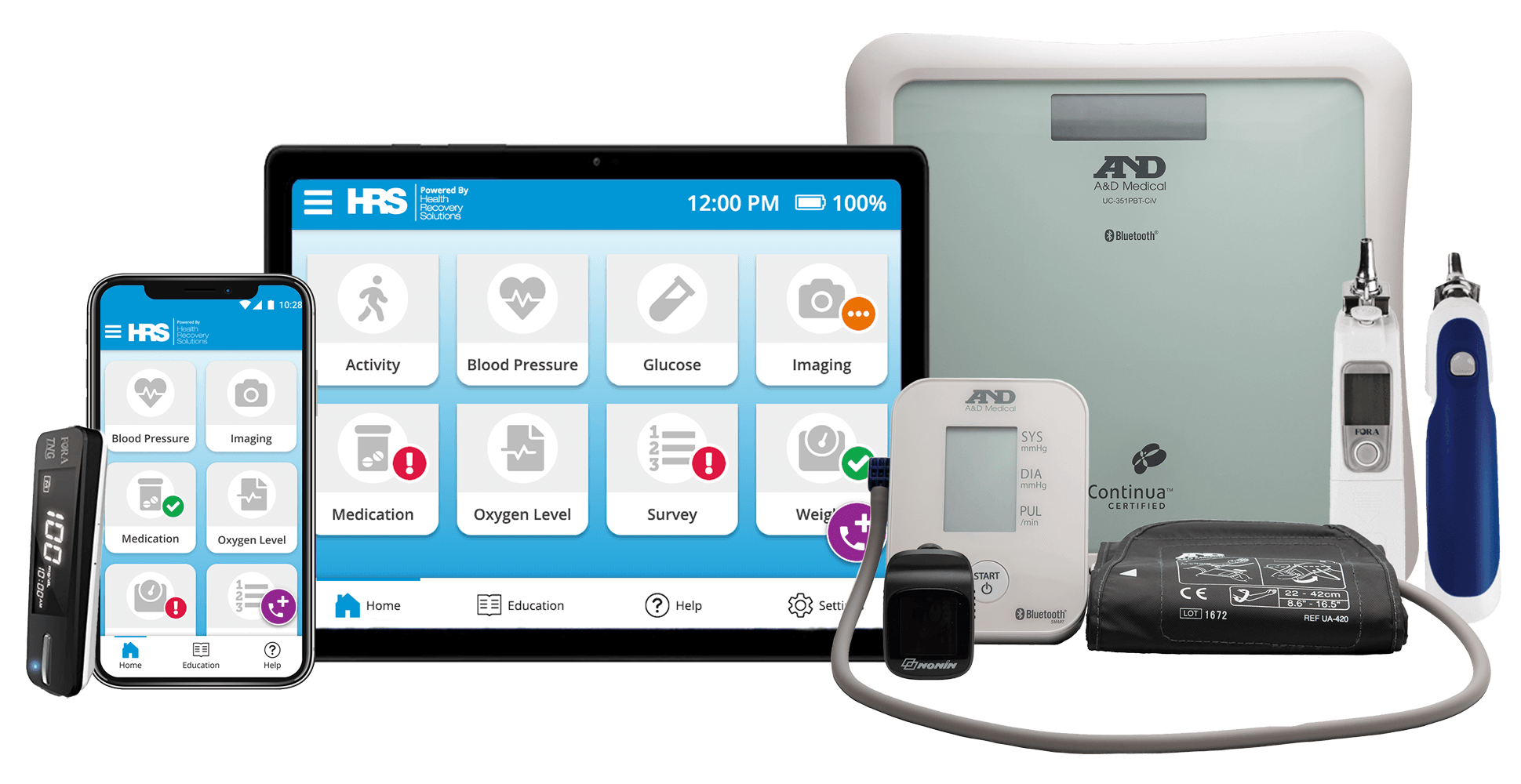
High-risk patients admitted to Home Health are enrolled in the RPM program and are typically monitored for at least a 30-day period. Patients receive either a tablet or access to the RPM platform via their personal smart device. In addition, patients are provided biometric monitoring devices with which to track their blood pressure, heart rate, weight, oxygen level, and potentially more.
During their enrollment period, patients are provided with an individual care plan and are expected to record their vital signs daily, respond to symptom surveys, and interact with educational videos and teach-back quizzes. All patient data is collected and reviewed daily by the CommonSpirit Health at Home team, enabling clinicians to triage patients, provide interventions as indicated to prevent adverse outcomes.
Remote patient monitoring interventions leveraged include:
Symptom Management
- Disease-specific symptom surveys are provided through the RPM platform
Biometric Monitoring
- Patients receive a set of biometric monitoring devices to record their vital signs (blood pressure, weight, oxygen levels, etc.) each day
- All biometric data is shared in real time with the CommonSpirit team, allowing for immediate evaluation of patients’ vitals and interventions if necessary
Medication Adherence
- Medication adherence is a key goal of the RPM program
- Patients receive medication reminders and are required to record their daily medication intake
- When patients do not indicate that their medication was taken, the CommonSpirit Health at Home team reaches out to them
HIPAA-compliant Virtual Visits
- Prioritized virtual visits, incorporating them into each patient’s plan of care
- Augmenting in-home visits with virtual visits leads to the cost savings that supports the RPM program
- Virtual visits are also utilized to triage patients when risk alerts are received
When it was time for us to expand our remote patient monitoring program, we were going to slowly roll this out over a six month period. Then it was March 2020, and we rolled it out in 14 states in two weeks, remotely. If you would have asked me if we could have done that, going forward, I would have said that is not the route we want to take. But because of the training capabilities that HRS afforded us, and being able to do a lot of these things remotely, we rolled it out and really made a difference in a lot of people's lives.
Rodney Plunkett
CommonSpirit Health at Home
Lower Acute Care Hospitalization Rate
Patients Monitored
of RPM Patients "Definitely Recommend" the Program
Results
Over one year between April 2020 and May 2021, CommonSpirit Health at Home’s program monitored over 2,800 patients between the ages of 1 to 103. Patients enrolled on the RPM program reported greater improvement than the global CommonSpirit Health at Home patient population across three criteria: ambulation, bathing, and pain management.
As COVID-19 cases and hospitalizations increased, CommonSpirit Health at Home partnered with an ACO to expand patient enrollment to manage a financially at-risk population. This partnership enabled CommonSpirit Health at Home to monitor a broad range of patients using RPM, specifically COVID-19 patients not eligible to receive home health services.
Additionally, CommonSpirit Health at Home began laying the foundation for a SNF at Home program prior to the COVID-19 PHE, but the need to provide facility-level care at home accelerated deployment of the new model of care. This program initially launched in communities across Omaha, Nebraska, targeting Medicare Shared Savings Program (MSSP) patients, including those with a COVID-19 diagnosis.