March 2020
Telehealth News:
Research & News Recap
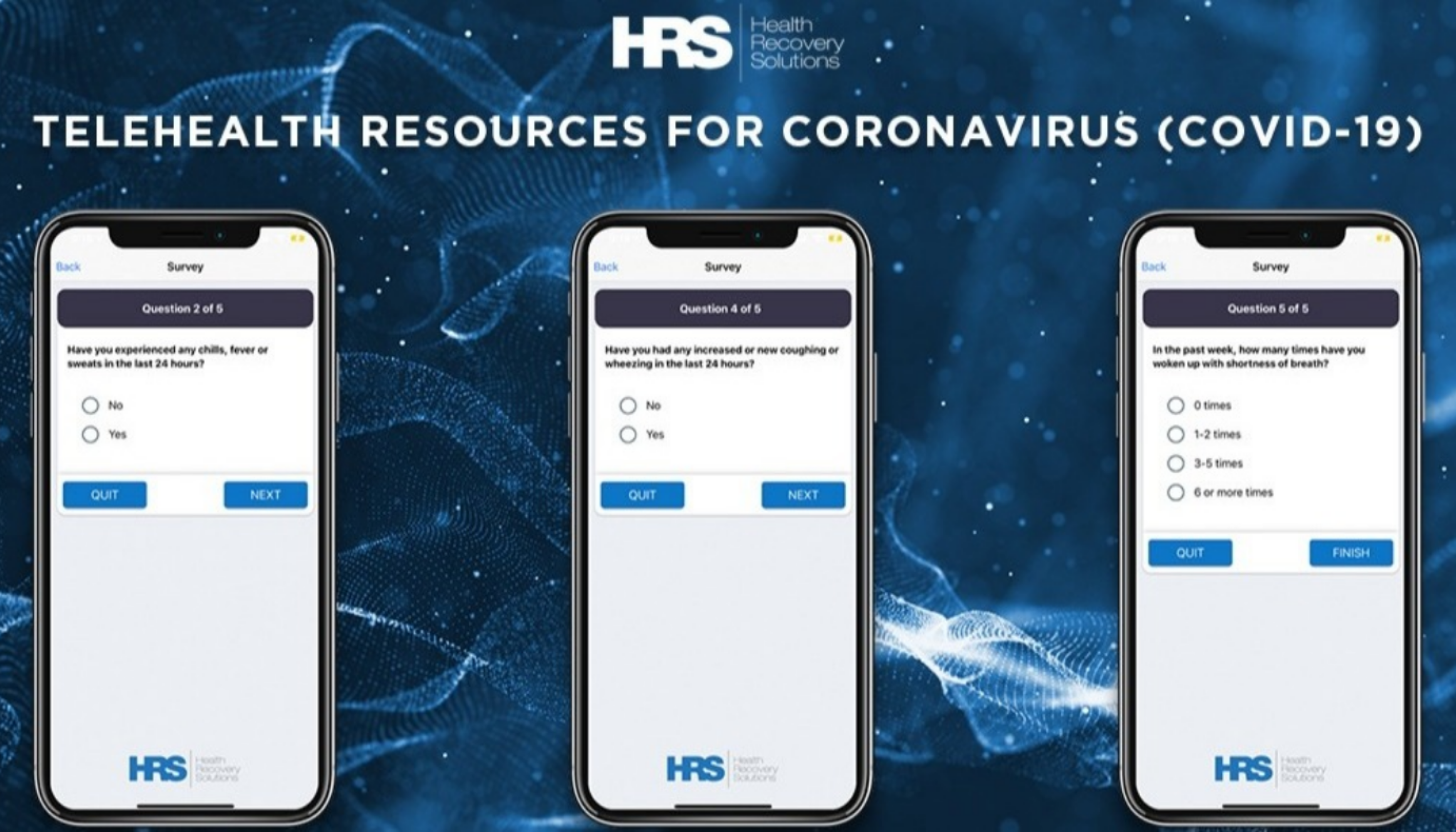
Interest in remote patient monitoring (RPM) and its positive impact has skyrocketed in the wake of the COVID-19 outbreak. Health systems and providers across the country are implementing expansive telehealth programs to enhance patient monitoring and disease management while reducing the strain of healthcare resources. Explore recent research on the efficacy of telehealth during the COVID-19 pandemic in HRS’ March 2020 Research & News Recap.
Part I. Research Findings - Remote Patient Monitoring and Telehealth
In this section, two studies conducted within the last few months demonstrate the benefits of utilizing RPM and telehealth to combat the outbreak of infectious diseases, such as COVID-19. Real quantitative and qualitative data from telehealth patients were collected, studied, and conclusions were drawn in the studies included below. The results point to the positive impacts of RPM on healthcare and the growth potential of telehealth.
Additionally, a virtual visits best practice article is included to shed light on how providers across the country are embracing video visits as they transition to remote care. In the article, four physicians discuss the challenges of implementing virtual visits across their clinics, as well as the benefits they've seen by doing so.
Article 1
The Current and Future Use of Telemedicine in Infectious Diseases Practice
What was studied?
In this literature review from October 2019, published just months before the widespread outbreak of COVID-19, Gregory and Coombes present the efficacy of using telehealth and remote patient monitoring (RPM) technologies to combat the spread of viruses. Coombes and Gregory begin with a historical summation of the use of telehealth and RPM to treat HIV, hepatitis C, tuberculosis, and STIs.
Following these evaluations, Gregory and Coombes focus on the present and future applications, which have greatly expanded as broadband access in remote areas has become widely available. Gregory and Coombes break down their evaluation into two keys areas in which telehealth and RPM have the largest impact on treatment of infectious diseases: home care and remote locations on the frontier of the outbreak. Adherence and biometric monitoring along with virtual visits enable clinicians to screen patients for infectious diseases during an outbreak, but telehealth and RPM also enables clinicians to monitor patients at-home during an outbreak to place fewer patients at risk and reduce community spread.
Research Findings
- HIV/AIDS: A review of 99 studies from 1996-2017 concluded that telehealth and RPM applications for HIV treatment improve clinic attendance rates and adherence to anti-retroviral therapy (ART) and reduce risky behavior
- STI Prevention: Telehealth has proven most beneficial to preventing further spread through virtual evaluations, prescriptions, and tests. The confidentiality provided by telehealth enables more people, particularly young adults most at-risk, to receive testing and proper treatment.
- Surgical Site Infection: Discharged patients at home face barriers to education and provider communication to monitor their wounds, placing them at higher risk for infection. Virtual visits have proven successful in the remote evaluation and monitoring of patient wound sites, allowing them to recover at home following a procedure and reduce their exposure risk.
- Tuberculosis: Video directly observed therapy (VDOT) enables patients to record drug therapy. The increased adherence has improved treatment for patients across income and resource levels in various countries. Long-term, this the increased adherence to medication and treatment (due to telehealth deployment) proves a promising resolution to treatment failure and drug resistance
- Rural and Limited Resource Settings: Recent innovations in health-tech have set the stage for remote diagnostic testing and screening for infectious diseases and viruses
Why do these findings matter?
In the event of a community outbreak or exacerbation in a patient’s long-term infection, timely access to healthcare providers and resources in essential. However, rural settings, underlying health conditions, and limited resources can prevent diagnosis and proper treatment of patients with infectious diseases or viruses as well as those at risk. We can see the unfortunate consequences of these roadblocks during the current COVID outbreak. However, what we have also seen during this crisis, is the resilience of our healthcare providers, adjusting at an organizational and individual level to monitor and treat COVID and non-COVID patients via telehealth and RPM.
Access the full article, here.
Date Published: October 2019
Coombes, Caitlin E, and Megan E Gregory. “The Current and Future Use of Telemedicine in Infectious Diseases Practice.” Current Infectious Disease Reports, U.S. National Library of Medicine, 19 Oct. 2019, www.ncbi.nlm.nih.gov/pubmed/31630276.
Article 2
Care of Patients with Pulmonary Arterial Hypertension during the Coronavirus (COVID-19) Pandemic
What was studied?
Pulmonary arterial hypertension (PAH) is a type of high blood pressure that affects over 200,000 Americans, damaging arteries in both the lungs and the right side of the heart. Diagnosis with PAH, as with many chronic conditions, requires patients to undergo significant lifestyle changes, further testing, and consistent appointments with their physician and other specialists. During the COVID-19 outbreak, individuals with existing pulmonary and cardiac diseases, including PAH patients, are at increased risk for adverse outcomes from COVID-19.
This increased risk combined with the specialty care necessary for the treatment and management of PAH, prompted physicians from the University of Utah Health to outline treatment options for PAH patients and providers utilizing telehealth and remote patient monitoring. Dr. John Ryan, et al. outline treatment balancing patients' exposure risk with the severity of the condition.
Common challenges:
- New Patients: Proper and expedient diagnosis of PAH given limited access to healthcare resources and testing as states have placed temporary holds on non-emergent procedures
- Established Clinically-Stable Patients: Though stable patients would ordinarily see their physicians for evaluation every three to six months, changes in the status of a PAH patient can occur rapidly and access to specialty physicians must be readily available should an exacerbation occur.
- Unstable Patients: A key concern during the outbreak is the misdiagnosed progression of PAH as most symptoms of an exacerbation mirror those of COVID.
Benefits experienced:
- New Patients: In the absence of advanced testing, educational materials delivered via telehealth are recommended to begin informing patients about the condition, its symptoms, and potential lifestyle changes they may need to undertake.
- Established Clinically-Stable Patients: Video conferencing and telephone calls are recommended for stable patients. Most patients being well-educated on their condition can accurately describe any symptoms or adverse effects of treatment via telephonic and video platforms.
- Unstable Patients: RPM is recommended to track patient status and monitor symptoms during the outbreak. Continuous monitoring of patients symptoms will enable clinicians to respond quickly to reported symptoms and trigger further evaluations and any necessary testing or treatment measures.
- Physician Collaboration: National PAH treatment centers can utilize telehealth to enhance coordination with regional and community centers. This improvement in communication will continue to benefit PAH patients after the corona virus has subsided.
Access the full article, here.
Date Published: March 2020
Ryan, John J, et al. “Care of Patients with Pulmonary Arterial Hypertension during the Coronavirus (COVID-19) Pandemic.” Sage Publishing, University of Utah Health, Mar. 2020, journals.sagepub.com/doi/pdf/10.1177/2045894020920153.
Article 3
Rapidly Converting to “Virtual Practices” - Outpatient Care in the Era of COVID-19
What was studied?
In this article, four physicians from Beth Israel Deaconess Medical Center, Children’s Hospital of Pittsburgh, Harvard University School of Public Health, and the University of Washington discuss their unique experiences with virtual visits during the COVID-19 pandemic.
The authors discuss their experience in trying to become “virtual practices” across four different primary care centers. They dive into their unique challenges and goals as the COVID-19 pandemic continues to develop.
Common challenges:
- Speed of transition to virtual care - providers are forced to embrace virtual care, under normal circumstances they’d have months to plan, test, and pilot
- Telephone care was easier to implement, video visits are taking longer to ramp up (the providers’ goal is to make video visits the norm as this will better replicate in-person care and increase likely payment)
- Internet capacity is negatively affecting video visits in some cases (dropped calls, poor image quality, lags) major themes emerged from the participant groups: care experience, emotions regarding pregnancy, privacy, and impact on daily life
Benefits experienced:
- Telehealth has allowed providers to continue to provide care even when quarantined themselves or having to stay home for child care or other circumstances
- Providers are avoiding exposure to their patients, and patients ar avoiding exposure to providers (and other patients) - this has proved especially important for patients with chronic disease and elderly patients
- For patients concerned that they have COVID-19, providers were able to address questions, coordinate testing, and triage symptoms via telehealth
- Patient’s have been relieved that they are able to visit their doctor through video - many were afraid to come into the office patients reported a growing sense of boredom and anxiety during their clinical admission - lack of privacy in the hospital was a major concern noted
Date Published: April 1, 2019
Mehrotra, Ateev, et al. “Rapidly Converting to ‘Virtual Practices’: Outpatient Care in the Era of Covid-19.” NEJM Catalyst Innovations in Care Delivery, 1 Apr. 2019, catalyst.nejm.org/doi/full/10.1056/CAT.20.0091.
Part II. Reimbursement Updates
Throughout the COVID-19 pandemic, the Centers for Medicare and Medicaid Services (CMS) have made changes to their policies in order to make telehealth more accessible across the country. Insights from our reimbursement team are included below.