November 2020
Telehealth News: Research & News Recap
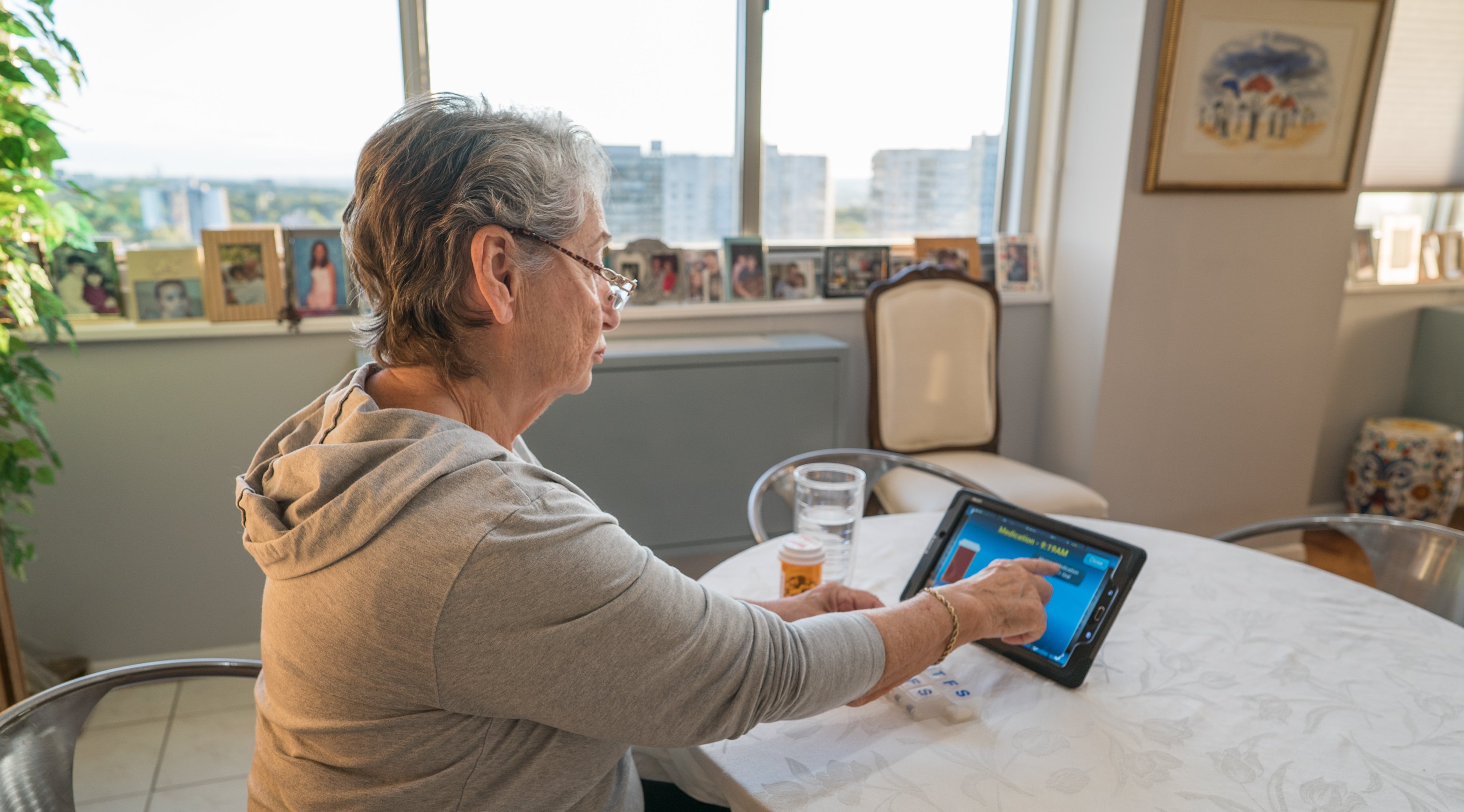
Interest in telehealth and remote patient monitoring (RPM) and its positive impact continues to grow as providers see the benefits of adding telehealth to their workflow, especially in response to the COVID-19 pandemic. This rise in adoption has led to increased and extensive research on telehealth and RPM programs as well as changes to government policies.
In addition to recent research on telehealth and RPM programs, you can explore recaps from Health Recovery Solutions’ Vision to Virtual event that occurred in October. You can access session recordings and article recaps below.
Part I. Research Findings - Remote Patient Monitoring and Telehealth
In this section, three studies conducted on various uses of telehealth and RPM are analyzed. Real quantitative and qualitative data from telehealth patients were collected, studied, and conclusions were drawn in the studies included below. The results point to the positive impacts of telehealth and RPM in healthcare in everyday use as well as during the COVID-19 pandemic.
Article 1
Impact on Readmission Reduction Among Heart Failure Patients Using Digital Health Monitoring: Feasibility and Adoptability Study
What was studied?
Heart failure (HF) affects approximately 6.2 million people in the United States and has a 5-year mortality rate of approximately 42%. Expected to exceed 8 million cases by 2030, it’s estimated that total annual HF costs will increase to nearly $70 billion in the same time period. Recently, many physicians and health systems have turned to telehealth and remote patient monitoring to broaden the scope of care in chronic disease management.The goal of this study, which was part of an ongoing program at Mount Sinai Hospital in New York City named the Heart Health Program, was to examine the feasibility of using digital health monitoring in real-world home settings. Researchers explored patient adoption of digital health and evaluated the impact on 30-day readmission rate. Vital sign data, including blood pressure (BP) and weight, were collected through an ambulatory remote monitoring system with a Bluetooth BP cuff and a digital scale.
Research Findings
The Heart Health Program enrolled a total of 60 patients into the study; two patients dropped out because of undisclosed personal reasons. Of the remaining 58 patients in the program, 33% were female and 67% were male, with a median age of 62 years. Of the 58 patients, 57 were on Medicare or Medicaid. A majority of patients (60%) had been hospitalized in the prior 12 months before discharge.
Overall, there were 6 hospital readmissions (10%) after 30 days, compared with the national 30-day readmission rate of 25%, this is a significant decrease; Mount Sinai Hospital’s readmission rate is noted at 23%. The 6 readmitted patients utilized BP and weight monitors less frequently than non-readmitted patients. Patients aged less than 70 years used the monitors more frequently on average.
Why do these findings matter?
As the total number of HF cases is expected to grow over the next 10 years, the cost. RPM and telehealth offer efficient ways to monitor HF patients at home and decrease their hospital readmissions rate. In turn, hospital readmission costs as well as symptom exacerbations will decline. Having access to condition education, patients will be able to better spot exacerbations and get ahead of them before needing to revisit the hospital. It gives them better control of their health and comfort in knowing they can handle their care management from home.
Access the full article, here.
Date Published: November 15 2019 19, 2020
Park C, Otobo E, Ullman J, Rogers J, Fasihuddin F, Garg S, Kakkar S, Goldstein M, Chandrasekhar SV, Pinney S, Atreja A. Impact on Readmission Reduction Among Heart Failure Patients Using Digital Health Monitoring: Feasibility and Adoptability Study. JMIR Med Inform 2019;7(4):e13353; DOI: 10.2196/13353
Article 2
Association of Continuous Assessment of Step Count by Remote Monitoring With Disability Progression Among Adults With Multiple Sclerosis
What was studied?
Over a one year period from June 2015 to August 2016, researchers at Weill Institute for Neurosciences studied the correlation between average daily step count and Multiple Sclerosis (MS) progression. MS is a leading cause of non-traumatic disability in the developed world, with walking impairment a major contributing factor. 95 patients were assigned to the study based on whether they had relapsing (flare-ups or attacks of inflammation) or progressive (steady worsening) MS and could walk unassisted for more than 2 minutes. Focusing on using remote patient monitoring (RPM) technology, researchers had participants wear an accelerometer to assess average continuous daily step count activity.
Research Findings
At the end of the 1-year study period, 79 individuals had completed the study - the withdrawal reasons included personal reasons, inability to synch devices, relocation, and cutaneous sensitivity. 63% of participants had relapsing MS, and 37% had progressive MS; 59 participants were women, and 36 participants were men. The mean age was 49.6 years (range, 22.0-74.0 years). The median disease duration was 13.0 years. The median daily step count for the entire cohort at baseline was 4,766.
Overall, it was found that step count reduction was associated with worsening of clinic-based and patient-reported outcomes and occurred even when conventional disability measures remained stable. In this study, patients with progressive MS were found to have significantly fewer average daily steps than did patients with relapsing MS. The continuous remote activity monitoring of individuals with MS appears to be feasible. The use of RPM technology, like the accelerometer, has given researchers a better understanding of the correlation between lack of walking and MS progression, and inevitably, difficulty walking as the disease continues to progress.
Why do these findings matter?
These results appear to support the use of average daily step count as a sensitive longitudinal outcome measure in MS and as a clinically relevant metric for targeted intervention and better treatment plans. Adjusting physical activity and rehabilitation for patients with MS are vital to the patients’ overall lifestyle. For patients with MS, treatments, medication, or rehab, make a huge difference in their condition progression. Using wearable accelerometers records how much a person actually moves in his or her daily life and gives clinicians a meaningful metric to better inform clinical care and neurologic rehabilitation.
Access the full article, here.Date Published: March 15, 2019
Block VJ, Bove R, Zhao C, et al. Association of Continuous Assessment of Step Count by Remote Monitoring With Disability Progression Among Adults With Multiple Sclerosis. JAMA Netw Open. 2019;2(3):e190570. doi:10.1001/jamanetworkopen.2019.0570
Article 3
Telehealth Uptake into Prenatal Care and Provider Attitudes during the COVID-19 Pandemic in New York City: A Quantitative and Qualitative Analysis
What was studied?
Over a 5-week period from March 9, 2020, to April 12, 2020, researchers at Columbia University Irving Medical Center and New York Presbyterian Morgan Stanley Children's Hospital of New York focused on their ambulatory prenatal care facilities and their transition to virtual visits during the COVID-19 pandemic. This study aimed to determine to what degree prenatal care could be transitioned to telehealth and to describe providers' experience with this transition.
Researchers examined prenatal care virtual visits over the 5-week period, which included 1-week of pre-implementation data; pre-implementation data determined the nature of the prenatal visits to be transitioned virtually (first and returning visits, postpartum visit, and preconception visits). After determining approved prenatal visits for participation in the study, a survey was given to providers that were providing routine prenatal care. This survey’s purpose was to determine the accessibility, efficiency, and effectiveness of virtual prenatal visits among the population studied.
Research findings
Data was collected from 4,248 pregnancy-related ambulatory visits including first prenatal care visits, return prenatal care visits, postpartum visits, consultations during pregnancy, and preconception consultations. Researchers evaluated the following types of practices providing prenatal care to transition to a virtual visit structure:
- Generalist obstetrics & gynecology faculty practice providing care to patients with commercial insurance.
- A maternal-fetal medicine (MFM) obstetrics and gynecology faculty practice providing care to patients with commercial insurance.
- A clinic system in Upper Manhattan providing prenatal care to a population with Medicaid insurance.
Overall, prenatal care providers found that the transition to telehealth for prenatal care increased access of care and provided adequate care to patients, improved efficiency of visits, saved time, and provided an extra layer of safety and protection to a vulnerable patient population. However, some patients with Medicaid faced difficulties in accessing telehealth visits versus women with commercial insurance providers due to Medicaid’s restrictions on virtual visits.
Why do these findings matter?
As pregnant women and patients with pre-existing conditions are at a higher-risk with COVID-19, it’s important that providers be flexible with the care they provide to reduce the risk of infection. As more providers and patients are seeing positive outcomes from the use of telehealth, more will leverage it as a resource to augment how they deliver care. The pandemic continues to affect how routine visits are scheduled and for at-risk patient populations, like pregnant women, virtual visits provide an extra layer of protection.
Access the full article, here.
Date Published: June 9, 2020
Madden, N., Emeruwa, U. N., Friedman, A. M., Aubey, J. J., Aziz, A., Baptiste, C. D., Coletta, J. M., D'Alton, M. E., Fuchs, K. M., Goffman, D., Gyamfi-Bannerman, C., Kondragunta, S., Krenitsky, N., Miller, R. S., Nhan-Chang, C. L., Saint Jean, A. M., Shukla, H. P., Simpson, L. L., Spiegel, E. S., Yates, H. S., … Ona, S. (2020). Telehealth Uptake into Prenatal Care and Provider Attitudes during the COVID-19 Pandemic in New York City: A Quantitative and Qualitative Analysis. American journal of perinatology, 37(10), 1005–1014. https://doi.org/10.1055/s-0040-1712939
Part II. Vision to Virtual Recap
Health Recovery Solutions’ Vision to Virtual is a forum for innovators, healthcare executives, telehealth users, and technology champions to discuss the role of telehealth and RPM in today’s healthcare continuum.
Vision to Virtual welcomed HRS clients and healthcare leaders from across the industry to network, brainstorm, and discuss how telehealth is revolutionizing healthcare.
Vision to Virtual Recap
Please find highlights and recaps from a few sessions below that cover topics discussed, speaker insights, and more.
- Optimizing Virtual Care: Virtual Visit Best Practices: speakers Kim Putnam of ProMedica Home Health Care and Mandy Johnson of Banner Home Health Care discussed the public health emergency and the shortcomings and limitations of current health care delivery systems. You can read the session recap here.
- Pivoting a Telehealth Program in Response to COVID-19: session speakers Donna Turlington of Liberty HomeCare & Hospice Services, Danielle Flynn of Penn Medicine, and Kelly Pollard of BayCare Home Care, discussed and expanded on topics relating to pivoting a telehealth program including their initial response to COVID-19, effects on patient populations, using HRS’ COVID Care and Recovery plans, and more. You can read the session recap here.
You can access the session recordings, here and the session FAQs here.