December 2020
Telehealth News: Research & News Recap
Interest in telehealth and remote patient monitoring (RPM) and its positive impact continues to grow as providers see the benefits of adding telehealth to their workflow, especially in response to the COVID-19 pandemic. This rise in adoption has led to increased and extensive research on telehealth and RPM programs as well as changes to government policies.
Explore recent research on the efficacy of telehealth and understand new rulings from the Center of Medicare and Medicaid Services (CMS) in HRS’ December 2020 News & Research Recap.
Part I. Research Findings - Telehealth and Remote Patient Monitoring
In this section, three studies conducted on various uses of telehealth and RPM are analyzed. Real quantitative and qualitative data from patients were collected, studied, and conclusions were drawn in the studies included below. The results point to the positive impacts of telehealth and RPM for oncology, pediatric surgery, and heart failure patients.
Article 1
Remote Home Monitoring of Older Surgical Cancer Patients: Perspective on Study Implementation and Feasibility
What was studied?
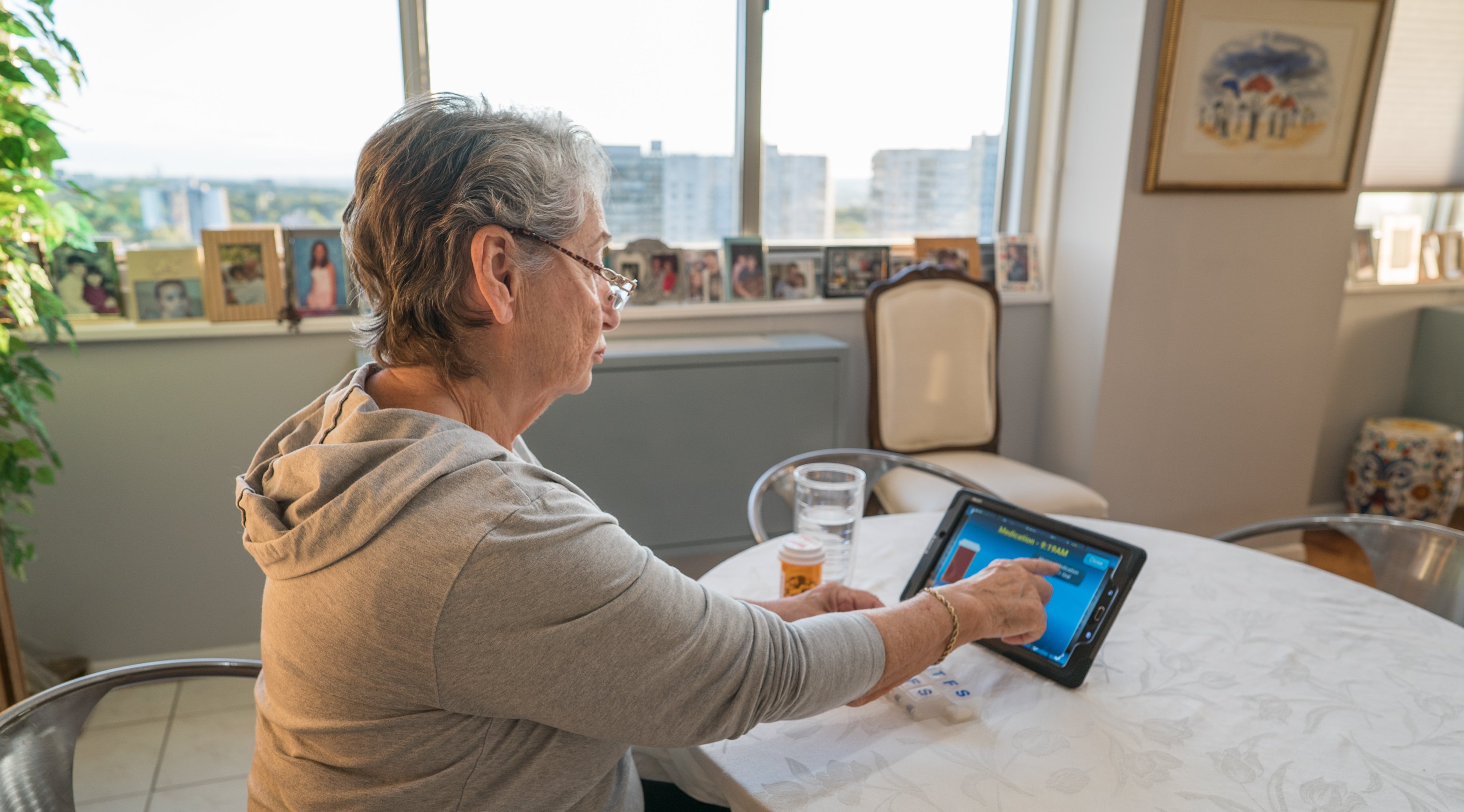
Over the past several years, Remote Patient Monitoring (RPM) has increased in popularity, now used as an alternative to care for oncology patients after hospital discharge. Some healthcare providers, however, are skeptical as to whether older patients will be receptive and adhere to the technology. This study assesses the feasibility - completion, compliance, acceptability, and usability - of post-op RPM for oncology patients older than 65 years.
This observational study recruited 47 patients aged 65 years or older who were scheduled for oncologic surgery. Patients used an activity tracker and mobile app to record their vitals before surgery and for 3 months post-op. They completed electronic health questionnaires 2 weeks after hospital discharge.
Research Findings
The patients in the study found postoperative home monitoring feasible, acceptable, and usable. Patients were compliant with wearing and synchronizing the physical activity tracker, and the study completion rate was high. Compliance rates for measurement of vital signs and completion of health questionnaires were lower than the average 85% from past studies, but were still acceptable.
Why do these findings matter?
The increasing amount of cancer diagnoses in patients older than 65 years is a global challenge. According to the study, newly diagnosed cancer is expected to increase from 7 million to 14 million cases by 2035. Because surgery is essential in more than 80% of new cancer cases, the total number of necessary surgeries will be approximately 17.3 million by 2030 - with multiple surgeries needed throughout treatment.
More than half of onco-geriatric patients experience at least one complication within 30 days after surgery - occurring more frequently after the patient has been discharged. Post-op RPM programs can not only measure vital signs with a high predictive value for hospitalization, but also detect immobilization and weight loss - both complication factors. With numbers expected to nearly double in the next 10 years, it’s important for oncologists to have telehealth and RPM measures in place to ensure their patients are safely recovering.
Access the full article, here.
Date Published: June 29, 2020
Jonker, L.T., Plas, M., de Bock, G.H. et al. Remote Home Monitoring of Older Surgical Cancer Patients: Perspective on Study Implementation and Feasibility. Ann Surg Oncol (2020). https://doi.org/10.1245/s10434-020-08705-1Article 2
Improving value and access to specialty medical care for families: a pediatric surgery telehealth program
What was studied?
In many parts of the world, access to pediatric specialty surgical services is often limited due to geographic, financial limitations, and/or inconvenience. To access care, families have to find a way to afford travel expenses, additional expenses, and time off from work and school. The purpose of this study was to evaluate a recently implemented pediatric surgical telehealth pilot program in British Columbia from the family and provider perspectives.
Between September 2014 and November 2017, 80 patients, averaged 7-years old, were seen in 19 remote telehealth centres - 23 as new referrals and 57 in follow-up consultation. The average travel distance avoided was 438 miles - most utilized mode of transport being air travel - with an estimated direct cost avoidance of $585. Patients from remote communities requiring new consultation or clinical follow-up were offered a telehealth alternative and were asked to provide feedback via a questionnaire. Provider satisfaction was also assessed via a questionnaire.
Research Findings
64 of the 80 families completed the questionnaire and 98% of those families indicated high overall satisfaction with the telehealth experience. Provider satisfaction was similarly high, in terms of both the technology user interface and clinical effectiveness. Families reported experiencing savings in travel time, school time missed and parental work time missed: without telehealth, families would have experienced an additional 5.35 hours of travel (1 way), 1 missed day of school for the child and 1 missed day of work for one or both parents. All families indicated limited issues with audio and visual clarity, as well as feeling comfortable throughout the virtual visit.
Why do these findings matter?
Aside from financial hardships, there are many factors that bring up hesitation with follow-up visits for geographically remote patients and their families. A major stress inducer is worrying about traveling with a post-op patient and the stress it can cause all family members. Spending less time traveling, and less time missing work and school, families can feel calmer and more secure in their recovery plans. Telehealth has obvious economic benefits to families. As the world continues to see changes in travel restrictions and procedures, it presents a better way for families to feel more confident that their child is still receiving high-level care.
Access the full article, here.Date Published: December 2019
Dean, P., O’Donnell, M., Zhou, L., & Skarsgard, E. D. (2019). Improving value and access to specialty medical care for families: a pediatric surgery telehealth program. Canadian journal of surgery. Journal canadien de chirurgie, 62(6), 436–441. https://doi.org/10.1503/cjs.005918
Article 3
Patients' and Nurses’ Experiences and Perceptions of Remote Monitoring of Implantable Cardiac Defibrillators in Heart Failure: Cross-Sectional, Descriptive, Mixed Methods Study
What was studied?
Linkoping University’s Department of Health, Medicine and Caring Sciences in Sweden studied the perceptions of patients and nurses who widely use and work with implantable cardioverter-defibrillators (ICDs) as remote monitoring peripherals. Researchers explored the experiences of both patients and nurses using RPM for ICD via questionnaires.
The study consisted of 175 heart failure (HF) patients from a single region in Sweden and 30 ICD nurses from various ICD clinics across the country. Patients were invited to complete an 8-question survey to assess their experiences with the ICDs; nurse experiences were also evaluated via an 8-question survey.
Research findings
Overall, more than 75% of both patients and nurses expressed their experience with RPM as being “very good”; however, the nurses noted more downsides than did the patients. Both patients and nurses found that RPM increased assurance, reliance, and safety. Patients found that RPM increased their own and their relatives’ sense of security and found the ICD RPM to be an advantage with fewer office-based visits.
Nurses found it difficult to handle different systems with different platforms, especially for smaller clinics with few patients. Another difficulty was setting the correct number of vital sign alarms for the individual patient. This caused a high number of transmissions bringing with it a risk of missing important information.
Why do these findings matter?
The number of patients treated with a primary ICD is increasing across the globe. Being able to closely monitor patients with heart failure can help reduce the risk of life-threatening symptoms or sudden cardiac death. Coupling monitoring and post-implant recovery with RPM gives patients a better sense of security knowing their health is being monitored. They’re able to be in close contact with their nurses and medical staff to ensure they’re recovering properly and adjusting their daily routines accordingly. Having this data from a patient helps nurses better understand how their organizational routine is functioning. They can make necessary adjustments and find the proper balance in achieving great results and admitting proper care.
Access the full article, here.
Date Published: September 28, 2020
Liljeroos M, Thylén I, Strömberg A Patients' and Nurses’ Experiences and Perceptions of Remote Monitoring of Implantable Cardiac Defibrillators in Heart Failure: Cross-Sectional, Descriptive, Mixed Methods Study. J Med Internet Res 2020;22(9):e19550
Part II. Reimbursement Update
Throughout the COVID-19 pandemic, the Centers for Medicare and Medicaid Services (CMS) have made changes to their policies in order to make telehealth more accessible across the country. As we continue to move forward, new federal policies and state laws have been proposed to continue expanding reimbursement for telehealth and RPM services. Below, you can review recent reimbursement updates.
Reimbursement Update
CMS Finalizes Telehealth, RPM Coverage in 2021 Physician Fee Schedule
CMS has released its 2021 Physician Fee Schedule on Medicare coverage for telehealth and RPM services. Building upon trends seen during this year's coronavirus pandemic, telehealth and RPM will see significant improvements in Medicare coverage in 2021. The 2021 Physician Fee Schedule aims to build upon the momentum for telehealth adoption. Some highlights are listed below:
- 60 new telehealth services that can be reimbursed under Medicare.
- Expanded coverage to new services and providers.
- Cover one nursing facility visit via telehealth every 14 days, down from once every 30 days.
- Expanded list of care providers able to be reimbursed for using telehealth to include clinical social workers, clinical psychologists, physical and occupational therapists and speech language pathologists.
- Coverage for direct supervision through real-time interactive audio-visual technology until the end of the PHE or 2021, whichever comes first.
Access the full article, here.
Date Published: December 2, 2020
Wicklund, Eric. “CMS Finalizes Telehealth, RPM Coverage in 2021 Physician Fee Schedule.” MHealthIntelligence, MHealthIntelligence, 2 Dec. 2020, https://mhealthintelligence.com/news/cms-finalizes-telehealth-rpm-coverage-in-2021-physician-fee-schedule.